Anti-inflammatory and Immunostimulant Therapy with Lactobacillus fermentum and Lactobacillus plantarum in COVID-19: A Literature Review
Abstract
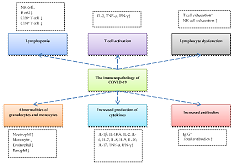
Inflammatory diseases are diseases characterized by inflammatory symptoms. Acute inflammatory disease can cause dysregulation of the inflammatory immune response, thereby inhibiting the development of protective immunity against infection. Among the acute inflammatory disease is COVID-19. The initial viral infection causes the antigen-presenting cells to detect the virus through a phagocytosis mechanism in the form of macrophage and dendritic cells. Lactobacillus fermentum and L. plantarum are gram-positive bacteria potentially serving as immunomodulators caused by inflammation and immune system response. Short-chain fatty acids (SCFA) produced by Lactobacillus can induce immune response through tolerogenic dendritic cells. This probiotic bacterium can induce the production of different cytokines or chemokines. Following the results of in vitro and in vivo tests, L. fermentum and L. plantarum can induce IL-10 release to activate regulatory T-cell and inhibit tumor necrosis factor-α (TNF-α) binding activity of nuclear factor kappa B (NF-κB). Literature review showed that dysregulation of inflammatory immune response disorders due to inflammatory disease could be treated using probiotic bacteria L. fermentum and L. plantarum. Therefore, it is necessary to conduct further studies on the potential of indigenous Indonesian strains of these two bacteria as anti-inflammatory and immunostimulants.
Full text article
References
2. Schultze JL, Aschenbrenner AC. COVID-19 and the human innate immune system. Cell. 2021;184(7):1671-92. doi:10.1016/j.cell.2021.02.029
3. Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. 2020;92(4):418-23. doi:10.1002/jmv.25681
4. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-33. doi:10.1056/nejmoa2001017
5. Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1-23. doi:10.1007/978-1-4939-2438-7_1
6. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (CoVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med. 2020;172(9):577-82. doi:10.7326/M20-0504
7. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-9. doi:10.1001/jama.2020.1585
8. Zhang B, Zhou X, Qiu Y, Song Y, Feng F, Feng J, et al. Clinical characteristics of 82 cases of death from COVID-19. PLoS One. 2020;15(7):e0235458. doi:10.1371/journal.pone.0235458
9. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the `Cytokine Storm' in COVID-19. J Infect. 2020;80(6):607-13. doi:10.1016/j.jinf.2020.03.037
10. Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and Multiorgan Response. Curr Probl Cardiol. 2020;45(8):100618. doi:10.1016/j.cpcardiol.2020.100618
11. Plaza-Díaz J, Ruiz-Ojeda FJ, Vilchez-Padial LM, Gil A. Evidence of the Anti-Inflammatory Effects of Probiotics and Synbiotics in Intestinal Chronic Diseases. Nutrients. 2017;9(6):555. doi:10.3390/nu9060555
12. Kim YA, Keogh JB, Clifton PM. Probiotics, prebiotics, synbiotics and insulin sensitivity. Nutr Res Rev. 2018;31(1):35-51. doi:10.1017/S095442241700018X
13. Freitas RHCN, Fraga CAM. NF-κB-IKKβ Pathway as a Target for Drug Development: Realities, Challenges and Perspectives. Curr Drug Targets. 2018;19(16):1933-42. doi:10.2174/1389450119666180219120534
14. Rocha-Ramírez LM, Pérez-Solano RA, Castañón-Alonso SL, Guerrero SSM, Pacheco AR, Garibay MG, et al. Probiotic Lactobacillus Strains Stimulate the Inflammatory Response and Activate Human Macrophages. J Immunol Res. 2017;2017:4607491. doi:10.1155/2017/4607491
15. Yang Y, Shen C, Li J, Yuan J, Wei J, Huang F, et al. Exuberant elevation of IP-10, MCP-3 and IL-1ra during SARS-CoV-2 infection is associated with disease severity and fatal outcome. J Allergy Clin Immunol. 2020;146(1):119-27. doi:10.1016/j.jaci.2020.04.027
16. Tajabadi N, Mardan M, Saari N, Mustafa S, Bahreini R, Manap MYA. Identification of Lactobacillus plantarum, Lactobacillus pentosus and Lactobacillus fermentum from honey stomach of honeybee. Braz J Microbiol. 2014;44(3):717-22. doi:10.1590/s1517-83822013000300008
17. Lee CS, Kim SH. Anti-inflammatory and Anti-osteoporotic Potential of Lactobacillus plantarum A41 and L. fermentum SRK414 as Probiotics. Probiotics Antimicrob Proteins. 2020;12(2):623-34. doi:10.1007/s12602-019-09577-y
18. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2):271-80.e8. doi:10.1016/j.cell.2020.02.052
19. Jia HP, Look DC, Shi L, Hickey M, Pewe L, Netland J, et al. ACE2 Receptor Expression and Severe Acute Respiratory Syndrome Coronavirus Infection Depend on Differentiation of Human Airway Epithelia. J Virol. 2005;79(23):14614-21. doi:10.1128/jvi.79.23.14614-14621.2005
20. Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:8. doi:10.1038/s41368-020-0074-x
21. Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631-7. doi:10.1002/path.1570
22. Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20(6):363-74. doi:10.1038/s41577-020-0311-8
23. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620-9. doi:10.1172/JCI137244
24. Gong J, Dong H, Xia QS, Huang ZY, Wang DK, Zhao Y, et al. Correlation analysis between disease severity and inflammation-related parameters in patients with COVID-19: a retrospective study. BMC Infect Dis. 2020;20(1):963. doi:10.1186/s12879-020-05681-5
25. Rabaan AA, Al-Ahmed SH, Muhammad J, Khan A, Sule AA, Tirupathi R, et al. Role of Inflammatory Cytokines in COVID-19 Patients: A Review on Molecular Mechanisms, Immune Functions, Immunopathology and Immunomodulatory Drugs to Counter Cytokine Storm. Vaccines. 2021;9(5):436. doi:10.3390/vaccines9050436
26. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-4. doi:10.1016/S0140-6736(20)30628-0
27. Schulert GS, Grom AA. Pathogenesis of macrophage activation syndrome and potential for cytokine- directed therapies. Annu Rev Med. 2015;66:145-59. doi:10.1146/annurev-med-061813-012806
28. Merad M, Martin JC. Author Correction: Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20(7):448. doi:10.1038/s41577-020-0353-y
29. Yang L, Liu S, Liu J, Zhang Z, Wan X, Huang B, et al. COVID-19: immunopathogenesis and Immunotherapeutics. Signal Transduct Target Ther. 2020;5(1):128. doi:10.1038/s41392-020-00243-2
30. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. doi:10.1016/S0140-6736(20)30183-5
31. Sulijaya B, Takahashi N, Yamazaki K. Lactobacillus-Derived Bioactive Metabolites for the Regulation of Periodontal Health: Evidences to Clinical Setting. Molecules. 2020;25(9):2088. doi:10.3390/molecules25092088
32. Villas-Bôas SG, Mas S, Akesson M, Smedsgaard J, Nielsen J. Mass spectrometry in metabolome analysis. Mass Spectrom Rev. 2005;24(5):613-46. doi:10.1002/mas.20032
33. Park SE, Yoo SA, Seo SH, Lee KI, Na CS, Son HS. GC–MS based metabolomics approach of Kimchi for the understanding of Lactobacillus plantarum fermentation characteristics. LWT Food Sci Technol. 2016;68:313-21. doi:10.1016/j.lwt.2015.12.046
34. Schummer C, Delhomme O, Appenzeller BMR, Wennig R, Millet M. Comparison of MTBSTFA and BSTFA in derivatization reactions of polar compounds prior to GC/MS analysis. Talanta. 2009;77(4):1473-82. doi:10.1016/j.talanta.2008.09.043
35. Chaudhary A, Verma K, Saharan BS. A GC-MS based metabolic profiling of probiotic lactic acid bacteria isolated from traditional food products. J Pure Appl Microbiol. 2020;14(1):657-72. doi:10.22207/JPAM.14.1.68
36. Vinolo MAR, Rodrigues HG, Hatanaka E, Sato FT, Sampaio SC, Curi R. Suppressive effect of short-chain fatty acids on production of proinflammatory mediators by neutrophils. J Nutr Biochem. 2011;22(9):849-55. doi:10.1016/j.jnutbio.2010.07.009
37. Liu Y, Alookaran JJ, Rhoads JM. Probiotics in autoimmune and inflammatory disorders. Nutrients. 2018;10(10):1537. doi:10.3390/nu10101537
38. Innes JK, Calder PC. Omega-6 fatty acids and inflammation. Prostaglandins Leukot Essent Fatty Acids. 2018;132:41-8. doi:10.1016/j.plefa.2018.03.004
39. Pathmakanthan S, Li CKF, Cowie J, Hawkey CJ. Lactobacillus plantarum 299: beneficial in vitro immunomodulation in cells extracted from inflamed human colon. J Gastroenterol Hepatol. 2004;19(2):166-73. doi:10.1111/j.1440-1746.2004.03181.x
40. Borthakur A, Anbazhagan AN, Kumar A, Raheja G, Singh V, Ramaswamy K, et al. The probiotic Lactobacillus plantarum counteracts TNF-{alpha}-induced downregulation of SMCT1 expression and function. Am J Physiol Gastrointest Liver Physiol. 2010;299(4):G928-34. doi:10.1152/ajpgi.00279.2010
41. Kim H, Jung BJ, Jung JH, Kim JY, Chung SK, Chung DK. Lactobacillus plantarum lipoteichoic acid alleviates TNF-α-induced inflammation in the HT-29 intestinal epithelial cell line. Mol Cells. 2012;33(5):479-86. doi:10.1007/s10059-012-2266-5
42. Kim HG, Lee SY, Kim NR, Lee HY, Ko MY, Jung BJ, et al. Lactobacillus plantarum lipoteichoic acid down-regulated Shigella flexneri peptidoglycan-induced inflammation. Mol Immunol. 2011;48(4):382-91. doi:10.1016/j.molimm.2010.07.011
43. Huang Y, Qu H, Liu D, Wa Y, Sang J, Yin B, et al. The effect of Lactobacillus fermentum DALI02 in reducing the oxidative stress and inflammatory response induced by high-fat diet of rats. RSC Adv. 2020;10(57):34396-402. doi:10.1039/d0ra05694d
44. Li S, Guo L, Si X, Dai Z, Zhou Z, Wu Z. Lactobacillus plantarum WCFS1 alleviates Aeromonas hydrophila NJ-1-induced inflammation and muscle loss in zebrafish (Danio rerio). Aquaculture. 2022;548(1):737603. doi:10.1016/j.aquaculture.2021.737603
45. Wu Y, Li X, Tan F, Zhou X, Mu J, Zhao X. Lactobacillus fermentum CQPC07 attenuates obesity, inflammation and dyslipidemia by modulating the antioxidant capacity and lipid metabolism in high-fat diet induced obese mice. J Inflamm. 2021;18(1):5. doi:10.1186/s12950-021-00272-w
46. Schultz M, Veltkamp C, Dieleman LA, Grenther WB, Wyrick PB, Tonkonogy SL, et al. Lactobacillus plantarum 299V in the treatment and prevention of spontaneous colitis in interleukin-10-deficient mice. Inflamm Bowel Dis. 2002;8(2):71-80. doi:10.1097/00054725-200203000-00001
47. Chytilová M, Mudroňová D, Nemcová R, Gancarčíková S, Buleca V, Koščová J, et al. Anti-inflammatory and immunoregulatory effects of flax-seed oil and Lactobacillus plantarum - BiocenolTM LP96 in gnotobiotic pigs challenged with enterotoxigenic Escherichia coli. Res Vet Sci. 2013;95(1):103-9. doi:10.1016/j.rvsc.2013.02.002
48. Kim W, Lee EJ, Bae IH, Myoung K, Kim ST, Park PJ, et al. Lactobacillus plantarum-derived extracellular vesicles induce anti-inflammatory M2 macrophage polarization in vitro. J Extracell Vesicles. 2020;9(1):1793514. doi:10.1080/20013078.2020.1793514
49. Yu P, Ke C, Guo J, Zhang X, Li B. Lactobacillus plantarum L15 Alleviates Colitis by Inhibiting LPS-Mediated NF-κB Activation and Ameliorates DSS-Induced Gut Microbiota Dysbiosis. Front Immunol. 2020;11:575173. doi:10.3389/fimmu.2020.575173
50. Kostelac D, Gerić M, Gajski G, Markov K, Domijan AM, Čanak I, et al. Lactic acid bacteria isolated from equid milk and their extracellular metabolites show great probiotic properties and anti-inflammatory potential. Int Dairy J. 2021;112:104828. doi:10.1016/j.idairyj.2020.104828
51. Chiu YH, Lu YC, Ou CC, Lin SL, Tsai CC, Huang CT, et al. Lactobacillus plantarum MYL26 induces endotoxin tolerance phenotype in Caco-2 cells. BMC Microbiol. 2013;13:190. doi:10.1186/1471-2180-13-190
52. Dos Santos TF, Melo TA, Almeida ME, Rezende RP, Romano CC. Immunomodulatory Effects of Lactobacillus plantarum Lp62 on Intestinal Epithelial and Mononuclear Cells. Biomed Res Int. 2016;2016:8404156. doi:10.1155/2016/8404156
53. Choi SH, Lee SH, Kim MG, Lee HJ, Kim GB. Lactobacillus plantarum CAU1055 ameliorates inflammation in lipopolysaccharide-induced RAW264.7 cells and a dextran sulfate sodium–induced colitis animal model. J Dairy Sci. 2019;102(8):6718-25. doi:10.3168/jds.2018-16197
54. Archer AC, Kurrey NK, Halami PM. In vitro adhesion and anti-inflammatory properties of native Lactobacillus fermentum and Lactobacillus delbrueckii spp. J Appl Microbiol. 2018;125(1):243-56. doi:10.1111/jam.13757
55. Rodríguez-Sojo MJ, Ruiz-Malagón AJ, Rodríguez-Cabezas ME, Gálvez J, Rodríguez-Nogales A. Limosilactobacillus fermentum CECT5716: Mechanisms and Therapeutic Insights. Nutrients. 2021;13(3):1016. doi:10.3390/nu13031016
56. Liu Z, Zhang P, Ma Y, Chen H, Zhou Y, Zhang M, et al. Lactobacillus plantarum prevents the development of colitis in IL-10-deficient mouse by reducing the intestinal permeability. Mol Biol Rep. 2011;38(2):1353-61. doi:10.1007/s11033-010-0237-5
57. Duary RK, Bhausaheb MA, Batish VK, Grover S. Anti-inflammatory and immunomodulatory efficacy of indigenous probiotic Lactobacillus plantarum Lp91 in colitis mouse model. Mol Biol Rep. 2012;39(4):4765-75. doi:10.1007/s11033-011-1269-1
58. Toshimitsu T, Mochizuki J, Ikegami S, Itou H. Identification of a Lactobacillus plantarum strain that ameliorates chronic inflammation and metabolic disorders in obese and type 2 diabetic mice. J Dairy Sci. 2016;99(2):933-46. doi:10.3168/jds.2015-9916
59. Ayyanna R, Ankaiah D, Arul V. Anti-inflammatory and Antioxidant Properties of Probiotic Bacterium Lactobacillus mucosae AN1 and Lactobacillus fermentum SNR1 in Wistar Albino Rats. Front Microbiol. 2018;9:3063. doi:10.3389/fmicb.2018.03063
60. Rodríguez-Nogales A, Algieri F, Garrido-Mesa J, Vezza T, Utrilla MP, Chueca N, et al. Differential intestinal anti-inflammatory effects of Lactobacillus fermentum and Lactobacillus salivarius in DSS mouse colitis: impact on microRNAs expression and microbiota composition. Mol Nutr Food Res. 2017;61(11):1700144. doi:10.1002/mnfr.201700144
61. Jang YJ, Kim WK, Han DH, Lee K, Ko G. Lactobacillus fermentum species ameliorate dextran sulfate sodium-induced colitis by regulating the immune response and altering gut microbiota. Gut Microbes. 2019;10(6):696-711. doi:10.1080/19490976.2019.1589281
62. Xia Y, Chen HQ, Zhang M, Jiang YQ, Hang XM, Qin HL. Effect of Lactobacillus plantarum LP-Onlly on gut flora and colitis in interleukin-10 knockout mice. J Gastroenterol Hepatol. 2011;26(2):405-11. doi:10.1111/j.1440-1746.2010.06498.x
63. Vilahur G, López-Bernal S, Camino S, Mendieta G, Padró T, Badimon L. Lactobacillus plantarum CECT 7315/7316 intake modulates the acute and chronic innate inflammatory response. Eur J Nutr. 2015;54(7):1161-71. doi:10.1007/s00394-014-0794-9
64. Ahn YS, Park MY, Shin JH, Kim JY, Kwon O. Lysate of Probiotic Lactobacillus plantarum K8 Modulate the Mucosal Inflammatory System in Dextran Sulfate Sodium-induced Colitic Rats. Korean J food Sci Anim Resour. 2014;34(6):829-35. doi:10.5851/kosfa.2014.34.6.829
65. Liu J, Gu Z, Song F, Zhang H, Zhao J, Chen W. Lactobacillus plantarum ZS2058 and Lactobacillus rhamnosus GG Use Different Mechanisms to Prevent Salmonella Infection in vivo. Front Microbiol. 2019;10:299. doi:10.3389/fmicb.2019.00299
66. Wang R, Zhou K, Xiong R, et al. Pretreatment with Lactobacillus fermentum XY18 Relieves Gastric Injury Induced by HCl/Ethanol in Mice via Antioxidant and Anti-Inflammatory Mechanisms. Drug Des Devel Ther. 2020;14:5721-34. doi:10.2147/DDDT.S280429
67. Kumar MKP, Halami PM, Peddha MS. Effect of Lactobacillus fermentum MCC2760-Based Probiotic Curd on Hypercholesterolemic C57BL6 Mice. ACS omega. 2021;6(11):7701-10. doi:10.1021/acsomega.1c00045
68. Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Therap Adv Gastroenterol. 2013;6(1):39-51. doi:10.1177/1756283X12459294
69. Gu S, Chen Y, Wu Z, Chen Y, Gao H, Lv L, et al. Alterations of the Gut Microbiota in Patients with Coronavirus Disease 2019 or H1N1 Influenza. Clin Infect Dis. 2020;71(10):2669-78. doi:10.1093/cid/ciaa709
70. Dang AT, Marsland BJ. Microbes, metabolites, and the gut-lung axis. Mucosal Immunol. 2019;12(4):843-50. doi:10.1038/s41385-019-0160-6
71. Nguyen QV, Chong LC, Hor YY, Lew LC, Rather IA, Choi SB. Role of Probiotics in the Management of COVID-19: A Computational Perspective. Nutrients. 2022;14(2):274. doi:10.3390/nu14020274
72. Menni C, Valdes AM, Freidin MB, Sudre CH, Nguyen LH, Drew DA, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med. 2020;26(7):1037-40. doi:10.1038/s41591-020-0916-2
73. Siedler S, Balti R, Neves AR. Bioprotective mechanisms of lactic acid bacteria against fungal spoilage of food. Curr Opin Biotechnol. 2019;56:138-46. doi:10.1016/j.copbio.2018.11.015
74. Suryani S, Purnawati Y, Putri SG, Rahmawati R, Yustitia A, Yusra Y. New Probiotic Isolation of Coconut Water’s Helpful Lactic Acid Bacteria Cure Covid-19 Patients. ARRUS J Eng Technol. 2022;2(1):1-11. doi:10.35877/jetech724
75. Li Q, Cheng F, Xu Q, Su Y, Cai X, Zeng F, et al. The role of probiotics in coronavirus disease-19 infection in Wuhan: A retrospective study of 311 severe patients. Int Immunopharmacol. 2021;95:107531. doi:10.1016/j.intimp.2021.107531
76. Gutiérrez-Castrellón P, Gandara-Martí T, Abreu AT, Nieto-Rufino CD, López-Orduña E, Jiménez-Escobar I, et al. Probiotic improves symptomatic and viral clearance in Covid19 outpatients: a randomized, quadruple-blinded, placebo-controlled trial. Gut Microbes. 2022;14(1):2018899. doi:10.1080/19490976.2021.2018899
77. Rather IA, Choi SB, Kamli MR, Hakeem KR, Sabir JSM, Park YH, et al. Potential Adjuvant Therapeutic Effect of Lactobacillus plantarum Probio-88 Postbiotics against SARS-COV-2. Vaccines. 2021;9(10):1067. doi:10.3390/vaccines9101067
Authors
Copyright (c) 2022 Harry Noviardi, Dyah Iswantini, Sri Mulijani, Setyanto Tri Wahyudi, Tatik Khusniati

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.