Identification of Drug-Related Problems in Hypertension Comorbid Type 2 Diabetes Mellitus Patients at Primary Health Care Center Batununggal District Bandung
Abstract
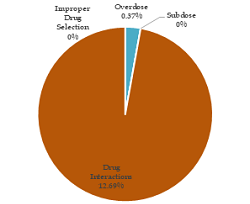
Many factors can increase the risk of hypertension, one of which is diabetes mellitus. The study aims to provide an overview of Drug-Related Problems (DRPs) in patients with hypertension comorbid type 2 diabetes mellitus at Primary Health Care Center Batununggal District Bandung. This research was an observational study with retrospective data collection and descriptive analysis. Data were taken from patient prescriptions January-December 2019 period. The sample inclusion criteria are patients aged 30-75 years, patients diagnosed with hypertension comorbid type 2 diabetes mellitus, and patients treated in January-December 2019. The number of samples that met the inclusion criteria was 268 patients, of which 69 patients (25.75%) are male, and 199 patients (74.25%) are female. 164 patients (61.2%) are aged 60-75 years old. It is found that 1 case (0.37%) has the drug-related problem of drug overdose and as many as 34 cases (12.69%) have potential drug interactions.
Full text article
References
2. Akalu Y, Belsti Y. Hypertension and Its Associated Factors Among Type 2 Diabetes Mellitus Patients at Debre Tabor General Hospital, Northwest Ethiopia. Diabetes Metab Syndr Obes. 2020;13:1621-31. doi:10.2147/DMSO.S254537
3. Ohishi M. Hypertension with diabetes mellitus: physiology and pathology. Hypertens Res. 2018;41(6):389-93. doi:10.1038/s41440-018-0034-4
4. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17:83. doi:10.1186/s12933-018-0728-6
5. Guerrero-García C, Rubio-Guerra AF. Combination therapy in the treatment of hypertension. Drugs Context. 2018;7:212531. doi:10.7573/dic.212531
6. Al-Azzam SI, Alzoubi KH, AbuRuz S, Alefan Q. Drug-related problems in a sample of outpatients with chronic diseases: a cross-sectional study from Jordan. Ther Clin Risk Manag. 2016;12:233-9. doi:10.2147/tcrm.s98165
7. Anshila MK, Nambiar DP, Augustine DV, Saseendran M, Shabraya AR, Siva S. Evaluation of Drug Related Problems in Patients with Chronic Disease at Tertiary Care Teaching Hospital. Int J Health Sci Res. 2020;10(9):144-55.
8. Septiani V, Sutjiatmo AB, Rustam LD. Identification of Drug-Related Problems (DRPs) Antihypertension on Hypertension Patient with Hyperlipidemia at One of Puskesmas in Bandung. In Asian Federation for Pharmaceutical Sciences (AFPS) 2019. Depok: Universitas Indonesia.
9. DiPiro JT, Yee GC, Posey M, Haines ST, Nolin TD, Ellingrod V. Pharmacotherapy: A Pathophysiologic Approach. 11th ed. New York: McGraw Hill Professional; 2020.
10. Ministry of Health Republic of Indonesia. Hasil Utama Riskesdas 2018. Jakarta: Health Research and Development Agency, Ministry of Health Republic of Indonesia; 2018.
11. Sabbatini AR, Kararigas G. Estrogen-related mechanisms in sex differences of hypertension and target organ damage. Biol Sec Differ. 2020;11:31. doi:10.1186/s13293-020-00306-7
12. Singh S, Shankar R, Singh GP. Prevalence and Associated Risk Factors of Hypertension: A Cross-Sectional Study in Urban Varanasi. Int J Hypertens. 2017;2017:5491838. doi:10.1155/2017/5491838
13. Nishiwaki M, Yonemura H, Kurobe K, Matsumoto N. Four weeks of regular static stretching reduces arterial stiffness in middle-aged men. Springerplus. 2015;4:555. doi:10.1186/s40064-015-1337-4
14. Qiu L, Wang W, Sa R, Liu F. Prevalence and Risk Factors of Hypertension, Diabetes, and Dyslipidemia among Adults in Northwest China. 2021;2021:5528007. doi:10.1155/2021/5528007
15. Yimama M, Jarso H, Desse TA. Determinants of drug-related problems among ambulatory type 2 diabetes patients with hypertension comorbidity in Southwest Ethiopia: a prospective cross sectional study. BMC Res Notes. 2018;11:679. doi:10.1186/s13104-018-3785-8
16. Tardy AL, Pouteau E, Marquez D, Yilmaz C, Scholey A. Vitamins and Minerals for Energy, Fatigue and Cognition: A Narrative Review of the Biochemical and Clinical Evidence. Nutrients. 2020;12(1):228. doi:10.3390/nu12010228
17. Moretti R, Caruso P. The Controversial Role of Homocysteine in Neurology: From Labs to Clinical Practice. Int J Mol Sci. 2019;20(1):231. doi:10.3390/ijms20010231
18. Tinelli C, Di Pino A, Ficulle E, Marcelli S, Feligioni M. Hyperhomocysteinemia as a Risk Factor and Potential Nutraceutical Target for Certain Pathologies. Front Nutr. 2019;6:49. doi:10.3389/fnut.2019.00049
19. Fu J, Liu Y, Zhang L, Zhou L, Li D, Quan H, et al. Nonpharmacologic Interventions for Reducing Blood Pressure in Adults with Prehypertension to Established Hypertension. J Am Heart Assoc. 2020;9(19):e016804. doi:10.1161/jaha.120.016804
20. Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and Control of Hypertension: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72(11):1278-93. doi:10.1016/j.jacc.2018.07.008
21. Mahmood S, Shah KU, Khan TM, Nawaz S, Rashid H, Baqar SWA, et al. Non-pharmacological management of hypertension: in the light of current research. Ir J Med Sci. 2019;188(2):437-52. doi:10.1007/s11845-018-1889-8
22. Fares H, DiNicolantonio JJ, O’Keefe JH, Lavie CJ. Amlodipine in hypertension: a first-line agent with efficacy for improving blood pressure and patient outcomes. Open Heart. 2016;3(2):e000473. doi:10.1136/openhrt-2016-000473
23. Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. A Comprehensive Review of Non-Steroidal Anti-Inflammatory Drug Use in The Elderly. Aging Dis. 2018;9(1):143-50. doi:10.14336/AD.2017.0306
24. Baxter, K. Stockley’s Drug Interactions. 8th ed. London: Pharmaceutical Press; 2008. p. 861-863.
25. George J, MacDonald T. Home Blood Pressure Monitoring. Eur Cardiol. 2015;10(2):95-101. doi:10.15420/ecr.2015.10.2.95
26. Garin N, Sole N, Lucas B, Matas L, Moras D, Rodrigo-Troyano A, et al. Drug related problems in clinical practice: a cross-sectional study on their prevalence, risk factors and associated pharmaceutical interventions. Sci Rep. 2021;11:883. doi:10.1038/s41598-020-80560-2
27. Farha RA, Saleh A, Aburuz S. The impact of drug related problems on health-related quality of life among hypertensive patients in Jordan. Pharm Pract. 2017;15(3):995. doi:10.18549/PharmPract.2017.03.995
28. Huri ZH, Wee HF. Drug related problems in type 2 diabetes patients with hypertension: a cross-sectional retrospective study. BMC Endocr Disord. 2013;13:2. doi:10.1186/1472-6823-13-2
Authors
Copyright (c) 2021 Vina Septiani, Pudjiastuti Kartidjo, Alfi Nurul Islamiyah, Abdul Aziz MSW, Iis Rukmawati

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.