Comparison of Pain Scale, Hemodynamics, and Side Effects of Percutaneous and Intravenous Fentanyl in Post Sectio Caesaria Patients at Bunda Hospital
Abstract
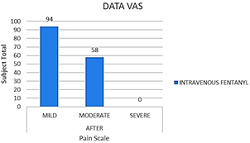
This is novel research about comparison pain scale, hemodynamics, and side effects of percutaneous and intravenous fentanyl in post sectio cesarean patients. Sectio cesarean is a method of delivering a fetus through an incision in the abdominal wall (laparotomy) and the uterus wall. This method induces pain in the incision, so patients feel complicated or afraid to mobilize. Fentanyl is one of the opioid analgesics, which is the main choice in section caesarian surgery because safe for breastfeeding, is more potent than morphine, and acts as balanced anesthesia—comparing the use of percutaneous fentanyl with intravenous fentanyl with pain scale parameters, hemodynamics, and side effects in sectio caesarian patients at Bunda Mother and Child Hospital Jakarta. Before conducting this research, an observational study first makes an ethical approval. Data were taken prospectively and collected simultaneously to compare percutaneous and intravenous fentanyl performed on post sectio cesarean patients with the physical status of the American Society of Anesthesiologists (ASA) I–II at Bunda Mother and Child Hospital Jakarta from September to November 2020. Comparative data observed were pain scale parameters, hemodynamics, and side effects after percutaneous fentanyl therapy or intravenous fentanyl therapy. Data were processed using SPSS 22 version and Microsoft Excell 2016. In conclusion, intravenous fentanyl is more effective in reducing pain scale and has more minor side effects than percutaneous fentanyl. There is no significant difference in hemodynamic parameters (p-value >0.05).
Full text article
References
2. Ministry of Health of the Republic of Indonesia. Riset Kesehatan Dasar 2018. Jakarta (ID): Ministry of Health of the Republic of Indonesia; 2018.
3. Gupta A, Kaur K, Sharma S, Goyal S, Arora S, Murthy RSR. Clinical aspects of acute post-operative pain management & its assessment. J Adv Pharm Technol Res. 2010;1(2):97-108.
4. Rosenblum A, Marsch LA, Joseph H, Portenoy RK. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16(5):405-16. doi:10.1037/a0013628
5. Machelska H, Celik MÖ. Advances in Achieving Opioid Analgesia Without Side Effects. Front Pharmacol. 2018;9:1388. doi:10.3389/fphar.2018.01388
6. Woodhouse A, Ward EM, Mather LE. Intra-subject variability in post-operative patient-controlled analgesia (PCA): is the patient equally satisfied with morphine, pethidine and fentanyl? Pain. 1999;80(3):545-53. doi:10.1016/s0304-3959(98)00247-4
7. Siswagama TA, Bagianto H, Laksono RM. Efek Pemberian Pre-emptive Fentanyl 25 μg terhadap Kejadian Batuk Setelah Bolus Fentanyl 2 μg/kg IV (Fentanyl Induced Cough). JAI (Jurnal Anestesiologi Indonesia). 2013;5(1):1-10. doi:10.14710/jai.v5i1.6419
8. Kizilcik N, Menda F, Bilgen S, Keskin O, Koner O. Effects of a fentanyl-propofol mixture on propofol injection pain: a randomized clinical trial. Korean J Anesthesiol. 2015;68(6):556-60. doi:10.4097/kjae.2015.68.6.556
9. Mulyawati I, Azam M, Ningrum DNA. Faktor Tindakan Persalinan Operasi Sectio Caesarea. KEMAS J Kesehatan Masyarakat. 2011;7(1):14-21. doi:10.15294/kemas.v7i1.1788
10. Purnomo DP, Mahmud, Uyun Y. Patient Controlled Analgesia (PCA) Post Operation. J Komplikasi Anestesi. 2015;2(2):95-111.
11. Abdolrazaghnejad A, Banaie M, Tavakoli 2, Safdari M, Rajabpour-Sanati A. Pain Management in the Emergency Department: a Review Article on Options and Methods. Adv J Emerg Med. 2018;2(4):e45. doi:10.22114/ajem.v0i0.93
12. Nalamachu S, Gudin J. Characteristics of Analgesic Patch Formulations. J Pain Res. 2020;13:2343-54. doi:10.2147/jpr.s270169
13. Bajaj S, Whiteman A, Brandner B. Transdermal drug delivery in pain management. Continuing Educ Anaesth Crit Care Pain. 2011;11(2):39-43. doi:10.1093/bjaceaccp/mkq054
14. Jeal W, Benfield P. Transdermal fentanyl. A review of its pharmacological properties and therapeutic efficacy in pain control. Drugs. 1997;53(1):109-38. doi:10.2165/00003495-199753010-00011
15. Lejus C, Schwoerer D, Furic I, Le Moing JP, Levron JC, Pinaud M. Fentanyl versus sefentanyl: plasma concentration during continuous epidural postoperative infusion in children. Br J Anaesth. 2000;85(4):615-7. doi:10.1093/bja/85.4.615
16. Yang J, Bauer BA, Wahner-Roedler DL, Chon TY, Xiao L. The modified WHO analgesic ladder: Is it appropriate for chronic non-cancer pain? J Pain Res. 2020;2020:411-7. doi:10.2147/JPR.S244173
17. Mirschberger V, von Deimling C, Heider A, Spadavecchia C, Rohrbach H, Zeiter S. Fentanyl Plasma Concentrations after Application of a Transdermal Patch in Three Different Locations to Refine Postoperative Pain Management in Rabbits. Animals. 2020;10(10):1778. doi:10.3390/ani10101778
18. Hoy SM, Keating GM. Fentanyl transdermal matrix patch (Durotep MT patch; Durogesic DTrans; Durogesic SMAT): in adults with cancer-related pain. Drugs. 2008;68(12):1711-21. doi:10.2165/00003495-200868120-00008
19. Bujedo BM. A Clinical Approach to Neuraxial Morphine for the Treatment of Postoperative Pain. Pain Res Treat. 2012;2012:612145. doi:10.1155/2012/612145
20. Rayburn WF, Rathke A, Leuschen MP, Chleborad J, Weidner W. Randomized comparison of meperidine and fentanyl during labor. Obstet and Gynecol. 1989;74(4):604-6.
21. Anderson D. A review of systemic opioids commonly used for labor pain relief. J Midwifery Womens Health. 2011;56(3):222-39.
22. Pathan H, Williams J. Basic opioid pharmacology: an update. Br J Pain. 2012;6(1):11-6. doi:10.1177/2049463712438493
23. Peng PW, Sandler AN. A review of the use of fentanyl analgesia in the management of acute pain in adults. Anesthesiology. 1999. 90(2):576-99. doi:10.1097/00000542-199902000-00034
24. Park S. Ideal Target Blood Pressure in Hypertension. Korean Circ J. 2019;49(11):1002-9. doi:10.4070/kcj.2019.0261
25. Yancey R. Anesthetic Management of the Hypertensive Patient: Part II. Anesth Prog. 2018;65(3):206-13. doi:10.2344/anpr-65-03-17
26. Dolinak D. Opioid Toxicity. Acad Forensic Pathol. 2017;7(1):19-35. doi:10.23907/2017.003
27. Reves JG, Glass PSA, Lubarsky DA. Nonbarbiturate intravenous anesthetics. In: Miller RD, editor. Anesthesia. 5th ed. New York: Churchill Livingstone; 2000. p. 228-72
28. Wickham A, Highton, D, Martin D, Pan T. Care of elderly patients: a prospective audit of the prevalence of hypotension and the use of BIS intraoperatively in 25 hospitals in London. Perioper Med. 2016;5:12. doi:10.1186/s13741-016-0036-1
29. Klamt JG, Vicente WV, Garcia LV, Ferreira CA. Effects of dexmedetomidine-fentanyl infusion on blood pressure and heart rate during cardiac surgery in children. Anesthesiol Res Pract. 2010;2010:869049. doi:10.1155/2010/869049
30. Laksono RM, Isngadi. Fentanyl Intratekal Mencegah Menggigil Pasca Anestesi Spinal pada Seksio Sesaria. J Kedokteran Brawijaya. 2012;27(1):51-5. doi:10.21776/ub.jkb.2012.027.01.9
31. Techanivate A, Rodanant O, Tachawattanawisal W, Somsiri T. Intrathecal fentanyl for prevention of shivering in cesarean section. J Med Assoc Thail. 2005;88(9):1214-21.
32. Nugroho AM, Uyun Y, Melati AC. Demam pada penggunaan analgesia persalinan epidural. J Anestesi Obstetri Indonesia; 2018;1(1):72-9. doi:10.47507/obstetri.v1i1.27
33. Gleeson NC, Nolan KM, Ford MR. Temperature, labour, and epidural analgesia. Lancet. 1989;2(8667):861–2. doi:10.1016/s0140-6736(89)93020-1
34. Amri P, Nahrini S, Hajian-Tilaki K, Hamidian M, Alipour SF, Hamidi SH, et al. Analgesic Effect and Hemodynamic Changes Due to Dexmedetomidine Versus Fentanyl During Elective Colonoscopy: A Double-Blind Randomized Clinical Trial. Anesth Pain Med. 2018;8(6):e81077. doi:10.5812/aapm.81077
35. Sun S, Wang J, Bao N, Chen Y, Wang J. Comparison of dexmedetomidine and fentanyl as local anesthetic adjuvants in spinal anesthesia: a systematic review and meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2017;11:3413-24. doi:10.2147/dddt.s146092
36. Iqbal M, Sudadi, Ngurah IG. TIVA (Total Intravenous Anesthesia). J Komplikasi Anestesi. 2014;2(1):61-72.
37. Solihat Y. Penggunaan Opioid sebagai Balans Anestesi pada Craniotomi Emergensi dengan Meningioma. JAI (Jurnal Anestesiologi Indonesia). 2013;5(2):124-31. doi:10.14710/jai.v5i2.6414
Authors
Copyright (c) 2022 Annisa`'a Nurillah Moesthafa, Achmad Riviq Said, Ros Sumarny, Yati Sumiyati

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.