Effect of Drug Information Service on Clinical Outcome of Patients with Type 2 Diabetes Mellitus in Padang, Indonesia
Abstract
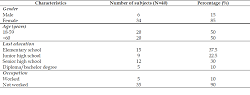
Type 2 diabetes mellitus (T2DM) has been a health burden worldwide, including Indonesia. However, T2DM therapy needs a long and complex process, which patients often do not favor, thus making them does not take medications as instructed and negatively affecting clinical outcomes. This study aimed to understand the effect of Drug Information Service provision on the clinical outcome of T2DM patients. This quasi-experimental study was conducted using one group pre-post-test design. As the clinical outcome, the fasting blood glucose levels were measured before and after the intervention. A drug information service was provided through direct explanation to the patients. Sociodemographic data were analyzed descriptively. The difference in fasting blood glucose before and after the intervention was assessed using Wilcoxon signed-rank test. Forty patients participated in this study. Most participants are female (N=34; 85%) and receive two-drugs combination therapy of metformin and sulfonylureas (N=32; 77.5%). Although there is a decrease in mean fasting blood glucose level after intervention (174.92±59.561 vs. 184.20±49.768), there is no significant difference between fasting blood glucose levels pre-intervention and post-intervention (p>0.05). It is concluded that despite the noticeable decline of blood glucose level after drug information service, its effect on blood glucose control is not significant.
Full text article
References
2. Soewondo P, Ferrario A, Tahapary DL. Challenges in diabetes management in Indonesia: a literature review. Global Health. 2013;9:63. doi:10.1186/1744-8603-9-63
3. Badan Penelitian dan Pengembangan Kesehatan. Laporan Nasional RISKESDAS 2018. Jakarta: Lembaga Penerbit Badan Penelitian dan Pengembangan Kesehatan; 2018. 198 p.
4. Chentli F, Azzoug S, Mahgoun S. Diabetes mellitus in elderly. Indian J Endocrinol Metab. 2015;19(6):744-52. doi:10.4103/2230-8210.167553
5. Hershon KS, Hirsch BR, Odugbesan O. Importance of Postprandial Glucose in Relation to A1C and Cardiovascular Disease. Clin Diabetes. 2019;37(3):250-9. doi:10.2337/cd18-0040
6. Chaudhury A, Duvoor C, Dendi VSR, Kraleti S, Chada A, Ravilla R, et al. Clinical Review of Antidiabetic Drugs: Implications for Type 2 Diabetes Mellitus Management. Front Endocrinol. 2017;8:6. doi:10.3389/fendo.2017.00006
7. Marín-Peñalver JJ, Martín-Timón I, Sevillano-Collantes C, Cañizo-Gómez FJD. Update on the treatment of type 2 diabetes mellitus. World J Diabetes. 2016;7(17):354-95. doi:10.4239/wjd.v7.i17.354
8. Alqarni AM, Alrahbeni T, Al Qarni A, Al Qarni HM. Adherence to diabetes medication among diabetic patients in the Bisha governorate of Saudi Arabia - a cross-sectional survey. Patient Prefer Adherence. 2018;13:63-71. doi:10.2147/ppa.s176355
9. Aloudah NM, Scott NW, Aljadhey HS, Araujo-Soares V, Alrubeaan KA, Watson MC. Medication adherence among patients with Type 2 diabetes: A mixed methods study. PLoS One. 2018;13(12):e0207583. doi:10.1371/journal.pone.0207583
10. Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence. 2016;10:1299-307. doi:10.2147/ppa.s106821
11. Verville L, Côté P, Grondin D, Mior S, Moodley K, Kay R, et al. Using technology-based educational interventions to improve knowledge about clinical practice guidelines. J Chiropr Educ. 2021;35(1):149-57. doi:10.7899/jce-19-17
12. Alexandra S, Handayani PW, Azzahro F. Indonesian hospital telemedicine acceptance model: the influence of user behavior and technological dimensions. Heliyon. 2021;7(12):e08599. doi:10.1016/j.heliyon.2021.e08599
13. Shrestha S, Shrestha R, Ahmed A, Sapkota B, Khatiwada AP, Christopher CM, et al. Impact of pharmacist services on economic, clinical, and humanistic outcome (ECHO) of South Asian patients: a systematic review. J Pharm Policy Pract. 2022;15(1):37. doi:10.1186/s40545-022-00431-1
14. Alamri SA, Al Jaizani RA, Naqvi AA, Al Ghamdi MS. Assessment of Drug Information Service in Public and Private Sector Tertiary Care Hospitals in the Eastern Province of Saudi Arabia. Pharmacy. 2017;5(3):37. doi:10.3390/pharmacy5030037
15. Rutter J, Rutter P. Impact of pharmacy medicine information service advice on clinician and patient outcomes: an overview. Health Info Libr J. 2019;36(4):299–317. doi: https://doi.org/10.1111/hir.12270
16. Gatwood JD, Chisholm-Burns M, Davis R, Thomas F, Potukuchi P, Hung A, et al. Impact of pharmacy services on initial clinical outcomes and medication adherence among veterans with uncontrolled diabetes. BMC Health Serv Res. 2018;18(1):855. doi:10.1186/s12913-018-3665-x
17. Negash Z, Berha AB, Shibeshi W, Ahmed A, Woldu MA, Engidawork E. Impact of medication therapy management service on selected clinical and humanistic outcomes in the ambulatory diabetes patients of Tikur Anbessa Specialist Hospital, Addis Ababa, Ethiopia. PLoS One. 2021;16(6):e0251709. doi:10.1371/journal.pone.0251709
18. Coutureau C, Slimano F, Mongaret C, Kanagaratnam L. Impact of Pharmacists-Led Interventions in Primary Care for Adults with Type 2 Diabetes on HbA1c Levels: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022;19(6):3156. doi:10.3390/ijerph19063156
19. Michiels Y, Bugnon O, Chicoye A, Dejager S, Moisan C, Allaert FA, et al. Impact of a Community Pharmacist-Delivered Information Program on the Follow-up of Type-2 Diabetic Patients: A Cluster Randomized Controlled Study. Adv Ther. 2019;36(6):1291–303. doi:10.1007/s12325-019-00957-y
20. Baker C, Retzik-Stahr C, Singh V, Plomondon R, Anderson V, Rasouli N. Should metformin remain the first-line therapy for treatment of type 2 diabetes? Ther Adv Endocrinol Metab. 2021;12:2042018820980225. doi:10.1177/2042018820980225
21. Kalra S, Das AK, Priya G, Ghosh S, Mehrotra RN, Das S, et al. Fixed-dose combination in management of type 2 diabetes mellitus: Expert opinion from an international panel. J Family Med Prim Care. 2020;9(11):5450-7. doi:10.4103/jfmpc.jfmpc_843_20
22. Ministry of Health Republic of Indonesia. Formularium Nasional. Jakarta: Ministry of Health Republic of Indonesia; 2017.
23. BPJS Kesehatan. Panduan Praktis Program Rujuk Balik Bagi Peserta JKN. Jakarta: BPJS Kesehatan; 2014.
24. Esti AB, Sandra C, Witcahyo E. Back-Referral Program in the Era of National Health Insurance at Balung District General Hospital of Jember in 2017. J Administrasi Kesehat Indones. 2019;7(1):33-9. doi:10.20473/jaki.v7i1.2019.33-39
25. Chen J, Wu C, Wang X, Yu J, Sun Z. The Impact of COVID-19 on Blood Glucose: A Systematic Review and Meta-Analysis. Front Endocrinol. 2020;11:574541. doi:10.3389/fendo.2020.574541
26. d'Emden M, McLeod D, Ungerer J, Appleton C, Kanowski D. Development of a fasting blood glucose-based strategy to diagnose women with gestational diabetes mellitus at increased risk of adverse outcomes in a COVID-19 environment. PLoS One. 2020;15(12):e0243192. doi:10.1371/journal.pone.0243192
27. Parrinello CM, Selvin E. Beyond HbA1c and glucose: the role of nontraditional glycemic markers in diabetes diagnosis, prognosis, and management. Curr Diab Rep. 2014;14(11):548. doi:10.1007/s11892-014-0548-3
28. Czupryniak L, Barkai L, Bolgarska S, Bronisz A, Broz J, Cypryk K, et al. Self-monitoring of blood glucose in diabetes: from evidence to clinical reality in Central and Eastern Europe--recommendations from the international Central-Eastern European expert group. Diabetes Technol Ther. 2014;16(7):460-75. doi:10.1089/dia.2013.0302
29. Tao J, Gao L, Liu Q, Dong K, Huang J, Peng X, et al. Factors contributing to glycemic control in diabetes mellitus patients complying with home quarantine during the coronavirus disease 2019 (COVID-19) epidemic. Diabetes Res Clin Pract. 2020;170:108514. doi:10.1016/j.diabres.2020.108514
30. Mamo Y, Bekele F, Nigussie T, Zewudie A. Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in Jimma University Medical Center, Jimma zone, south west Ethiopia: a case control study. BMC Endocr Disord. 2019;19(1):91. doi:10.1186/s12902-019-0421-0
31. American Diabetes Association. 6. Glycemic Targets: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(Suppl 1):S61-70. doi:10.2337/dc19-s006
32. Abubakar M, Atif M. Impact of Pharmacist-Led Interventions on Diabetes Management at a Community Pharmacy in Pakistan: A Randomized Controlled Trial. Inquiry. 2021;58:469580211036283. doi:10.1177/00469580211036283
33. David EA, Soremekun RO, Abah IO, Aderemi-Williams RI. Impact of pharmacist-led care on glycaemic control of patients with uncontrolled type 2 diabetes: A randomised controlled trial in Nigeria. Pharm Pract. 2021;19(3):2402. doi:10.18549/pharmpract.2021.3.2402
34. Sauriasari R, Sakti RM. Impact of a pharmacist-led patient education initiative on glycemic control of patients with type 2 diabetes mellitus: A single-center experience in West Jakarta, Indonesia. Int J Appl Pharm. 2018;10(1):252–6. doi:10.22159/ijap.2018.v10s1.56
35. Wibowo MINA, Setiawan D, Ikhwaniati ND, Sukma FA. Pengaruh Konseling dan Alat Bantu Pengingat Pengobatan terhadap Kepatuhan Minum Obat dan Outcome Klinik Pasien Diabetes Melitus dan Hipertensi. J Ilmu Kefarmasian Indones. 2020;18(2):169–76. doi:10.35814/jifi.v18i2.761
36. Insani WN, Lestari K, Abdulah R, Ghassani SK. Pengaruh Pelayanan Informasi Obat terhadap Keberhasilan Terapi Pasien Diabetes Melitus Tipe 2. J Farm Klin Indones. 2013;2(4):127–35.
37. Wireno EHD, Setiawan AA, Hendrianingtyas M, Pramudo SG. Factors Affecting Glycemic Control in Diabetes Mellitus Patients. Sains Med J Kedokt Kesehat. 2021;12(2):1-9. doi:10.30659/sainsmed.v12i2.7620
38. Kakade AA, Mohanty IR, Rai S. Assessment of factors associated with poor glycemic control among patients with Type II Diabetes mellitus. Integr Obes Diabetes. 2018;4(3):1–6. doi:10.15761/IOD.1000209
Authors
Copyright (c) 2022 Lailaturrahmi Lailaturrahmi, Fuji Araswati, Armenia Armenia, Rahmi Yosmar

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.