Quality of Life in End-Stage Renal Disease Patients Undergoing Hemodialysis and Its Affecting Factors in a Hemodialysis Unit of General Hospital Denpasar
Abstract
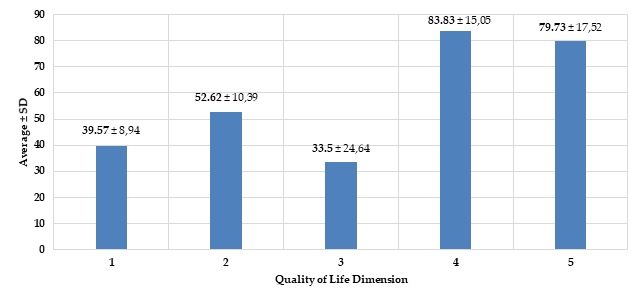
End-stage renal disease (ESRD) patients undergoing hemodialysis (HD) repeatedly can affect their quality of life (QOL). Its QOL value can vary according to the patient's characteristics amid health conditions that may make it difficult for them. This study aimed to analyze the QOL of ESRD patients undergoing HD and its affecting factors. This cross-sectional study was conducted in a Hemodialysis Outpatient Unit of General Hospital, Denpasar, Bali, from April to May 2021. A sample of 103 respondents was obtained by using the purposive sampling technique. Inclusion criteria were ESRD patients undergoing HD aged ≥8 years old, completing questionnaires thoroughly, and communicating well. Data was collected through the KDQOL-36 questionnaire to measure the QOL and medical records for completeness of patient identities. Data were analyzed using Spearman's ρ, η, Mann-Whitney, and an Independent sample t-test (CI 95%). Findings showed the majority of respondents were aged <60 years (75.7%), had secondary education (41.7%), were working (50.5%), were diagnosed with ESRD, and undergoing HD <3 Years (81.6%), the duration of each HD >4 hours (85.4%), three times a week (91.3%), having a BMI >29 kg/m2 (89.3%), and hypertension (42.7%). The respondents experienced major problems in their QOL on the burden of ESRD (33.50±24.64), physical (39.57±8.94), and mental component summary (52.62±10.39) dimensions. Respondent's characteristics, including education level, duration of each HD, and diagnosis with ESRD undergoing HD, contributed to their QOL (p <0.05). The patient's QOL needs to be improved through the family and health worker's support.
Full text article
References
2. Hustrini NM, Susalit E, Rotmans JI. Prevalence and risk factors for chronic kidney disease in Indonesia: An analysis of the National Basic Health Survey 2018. J Glob Health. 2022;12:04074. doi:10.7189/jogh.12.04074
3. National Kidney Foundation. KDOQI Clinical Practice Guideline for Diabetes and CKD: 2012 Update. Am J Kidney Dis. 2012;60(5):850-86. doi:10.1053/j.ajkd.2012.07.005
4. Rasyid H, Kasim H, Zatalia SR, Sampebuntu J. Quality of Life in Patients with Renal Failure Undergoing Hemodialysis. Acta Med Indones. 2022;54(2):307-13.
5. Mushtaque I, Awais-E-Yazdan M, Zahra R, Anas M. Quality of Life and Illness Acceptance among End-Stage Renal Disease (ESRD) Patients on Hemodialysis: The Moderating Effect of Death Anxiety during COVID-19 pandemic. Omega. 2022;7:302228221075202. doi:10.1177/00302228221075202
6. Barzegar H, Jafari H, Charati JY, Esmaeili R. Relationship Between Duration of Dialysis and Quality of Life in Hemodialysis Patients. Iran J Psychiatry Behav Sci. 2017;11(4):e6409. doi:10.5812/ijpbs.6409
7. Sumantrie P. Tingkat Kualitas Hidup Pasien Gagal Ginjal Kronik yang Menjalani Hemodialisa. Excellent Midwifery J. 2018;1(1):31–8. doi:10.55541/emj.v1i1.23
8. Manavalan M, Majumdar A, Kumar KTH, Priyamvada PS. Assessment of Health-Related Quality of Life and its Determinants in Patients with Chronic Kidney Disease. Indian J Nephrol. 2017;27(1):37–43. doi:10.4103/0971-4065.179205
9. Ravindran A, Sunny A, Kunnath RP, Divakaran B. Assessment of Quality of Life Among End-Stage Renal Disease Patients Undergoing Maintenance Hemodialysis. Indian J Palliat Care.2020;26(1):47-53.doi:10.4103/IJPC.IJPC_141_19
10. Aryzki S, Wanda MNR, Susanto Y, Saputera MMA, Putra AMP, Karani. Pengukuran Kualitas Hidup Pasien Hemodialisis Gagal Ginjal Kronik Di RSUD Ulin Banjarmasin Menggunakan Instrumen EQ-5D-5L. J Ilmiah Ibnu Sina. 2019;4(1):210–24. doi:10.36387/jiis.v4i1.230
11. Dewi NMPP, Loekman JS, Widiana IGR, Kandarini Y. Perbandingan Health-Related Quality of Life (HRQoL) Antara Penderita Penyakit Ginjal Kronik Dengan Non Penyakit Ginjal Kronik Pada Penduduk Asli Desa Pedawa Buleleng Bali. Medicina. 2018;49(3):443-8. doi:10.15562/medicina.v49i3.343
12. Sriandari LPF, Lesmana CBJ. Hubungan Depresi Dan Kualitas Hidup Pasien Penyakit Ginjal Kronik Yang Menjalani Hemodialisis di Bali 2015. E-Jurnal Medika Udayana. 2019;8(5):1-9.
13. Dewi IGAPA, Parut AA. Penyulit Dominan yang Dialami Selama Intradialisis pada Pasien yang Menjalani Terapi Hemodialisis di BRSU Tabanan-Bali. J Riset Kesehatan Nasional. 2019;3(2):56-61. doi:10.37294/jrkn.v3i2.173
14. Supriyadi R, Rakhima F, Gondodiputro RS, Darmawan G. Validity and Reliability of the Indonesian Version of Kidney Disease Quality of Life (KDQOL-36) Questionnaire in Hemodialysis Patients at Hasan Sadikin Hospital, Bandung, Indonesia. Acta Med Indones. 2019;51(4):318–23.
15. Cohen DE, Lee A, Sibbel S, Benner D, Brunelli SM, Tentori F. Use of the KDQOL-36TM for Assessment of Health-Related Quality of Life Among Dialysis Patients in The United States. BMC Nephrol. 2019;20(1)112. doi:10.1186/s12882-019-1295-0
16. Dewi NPRA, Kandarini Y, Sajinadiyasa IGK, Triharnoto T. Assessment of Quality of Life Among Chronic Kidney Disease Patients Undergoing Hemodialysis in Sanglah General Hospital, Denpasar From April-May 2017 Using EQ-5D-5L Questionnaire. Intisari Sains Medis. 2020;11(1):104-7. doi:10.15562/ism.v11i1.172
17. Adiningrum N, Andayani TM, Kristina SA. Analisis Faktor Klinik terhadap Kualitas Hidup Pasien Hemodialisis di RSUD dr. Loekmono Hadi Kudus. J Farmasi Ilmu Kefarmasian Indones. 2021;8(1):29-37. doi:10.20473/jfiki.v8i12021.29-37
18. van der Burgh AC, Rizopoulos D, Ikram MA, Hoorn EJ, Chaker L. Determinants of the Evolution of Kidney Function with Age. Kidney Int Rep. 2021;6(12):3054–63. doi:10.1016/j.ekir.2021.10.006
19. Sheen YJ, Sheu WH. Risks of Rapid Decline Renal Function in Patients with Type 2 Diabetes. World J Diabetes. 2014;5(6):835-46. doi:10.4239/wjd.v5.i6.835
20. Ipo A, Aryani T, Suri M. Hubungan Jenis Kelamin dan Frekuensi Hemodialisa DENGAN Kualitas Hidup Pasien Gagal Ginjal Kronik yang Menjalani Hemodialisa di Rumah Sakit Umum Daerah Raden Mattaher Jambi. J Akademika Baiturrahim Jambi. 2016;5(2):46–55. doi:10.36565/jab.v5i2.7
21. Ma HY, Chen S, Du Y. Estrogen and estrogen receptors in kidney diseases. Ren Fail. 2021;43(1):619-42. doi:10.1080/0886022x.2021.1901739
22. Medina D, Mehay D, Arnold AC. Sex differences in cardiovascular actions of the renin-angiotensin system. Clin Auton Res. 2020;30(5):393-408. doi:10.1007/s10286-020-00720-2
23. Fatonah L, Andayani TM, Yasin NM. Hubungan antara Efektivitas Hemodialisis dengan Kualitas Hidup Pasien Penyakit Ginjal Kronis di Yogyakarta. J Farmasi Ilmu Kefarmasian Indones. 2021;8(1):22–8. doi:10.20473/jfiki.v8i12021.22-28
24. Akbari AS, Cheraghi MA, Kazemnejad A, Nomali M, Zakerimoghadam M. Effect of Illness Perception Correction - Based Educational Program on Quality of Life and Self- Care in Patients with Heart Failure: a Randomized Controlled Trial. J Caring Sci. 2019;8(2):89-93. doi:10.15171/jcs.2019.013
25. Andermann A, CLEAR Collaboration. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016;188(17-18):E474-83. doi:10.1503/cmaj.160177
26. Bello AK, Okpechi IG, Osman MA, Cho Y, Htay H, Jha V, et al. Epidemiology of haemodialysis outcomes. Nat Rev Nephrol. 2022;18(6):378-95. doi:10.1038/s41581-022-00542-7
27. Cha J, Han D. Health-Related Quality of Life Based on Comorbidities Among Patients with End-Stage Renal Disease. Osong Public Health Res Perspect. 2020;11(4):194-200. doi:10.24171/j.phrp.2020.11.4.08
28. Hall ME, do Carmo JM, da Silva AA, Juncos LA, Wang Z, Hall JE. Obesity, hypertension, and chronic kidney disease. Int J Nephrol Renovasc Dis. 2014;7:75-88. doi:10.2147/ijnrd.s39739
29. Kustimah, Siswadi AGP, Djunaidi A, Iskandarsyah A. Quality of Life among Patients Undergoing Haemodialysis in Bandung: A Mixed Methods Study J Keperawatan Padjadjaran. 2020;8(1):84-92. doi:10.24198/jkp.v8i1.1330
30. Cox KJ, Parshall MB, Hernandez SHA, Parvez SZ, Unruh ML. Symptoms among patients receiving in-center hemodialysis: A qualitative study. Hemodial Int. 2017;21(4):524-33. doi:10.1111/hdi.12521
31. Jankowska-Polańska B, Uchmanowicz I, Wysocka A, Uchmanowicz B, Lomper K, Fal AM. Factors Affecting the Quality of Life of Chronic Dialysis Patients. Eur J Public Health. 2017;27(2):262-7. doi:10.1093/eurpub/ckw193
32. Medrano-Ureña MDR, Ortega-Ruiz R, Benítez-Sillero JdD. Physical Fitness, Exercise Self-Efficacy, and Quality of Life in Adulthood: A Systematic Review. Int J Environ Res Public Health. 2020;17(17):6343. doi:10.3390/ijerph17176343
33. Zyoud SH, Daraghmeh DN, Mezyed DO, Khdeir RL, Sawafta MN, Ayaseh NA, et al. Factors Affecting Quality of Life in Patients on Haemodialysis: A Cross-Sectional Study from Palestine. BMC Nephrol. 2016;17:44. doi:10.1186/s12882-016-0257-z
34. Wahyuni P, Miro S, Kurniawan E. Hubungan Lama Menjalani Hemodialisis dengan Kualitas Hidup Pasien Penyakit Ginjal Kronik dengan Diabetes Melitus di RSUP Dr. M Djamil Padang. J Kesehatan Andalas. 2018;7(4):480-5. doi:10.25077/jka.v7i4.905
35. Tchape ODM, Tchapoga YB, Atuhaire C, Proebe G, Cumber SN. Physiological and psychosocial stressors among hemodialysis patients in the Buea Regional Hospital, Cameroon. Pan Afr Med J. 2018;30:49. doi:10.11604/pamj.2018.30.49.15180
36. Finnegan-John J, Thomas VJ. The psychosocial experience of patients with end-stage renal disease and its impact on quality of life: findings from a needs assessment to shape a service. ISRN Nephrol. 2012;2013:308986. doi:10.5402/2013/308986
37. Garg AX, Suri RS, Eggers P, Finkelstein FO, Greene T, Kimmel PL, et al. Patients Receiving Frequent Hemodialysis Have Better Health-Related Quality of Life Compared to Patients Receiving Conventional Hemodialysis. Kidney Int. 2017;91(3):746-54. doi:10.1016/j.kint.2016.10.033
38. Sahathevan S, Khor BH, Ng HM, Gafor AHA, Daud ZAM, Mafra D, et al. Understanding Development of Malnutrition in Hemodialysis Patients: A Narrative Review. Nutrients. 2020;12(10):3147. doi:10.3390/nu12103147
39. Bollenbecker S, Czaya B, Gutiérrez OM, Krick S. Lung-kidney interactions and their role in chronic kidney disease-associated pulmonary diseases. Am J Physiol Lung Cell Mol Physiol. 2022;322(5):L625-40. doi:10.1152/ajplung.00152.2021
40. Flythe JE, Curhan GC, Brunelli SM. Shorter Length Dialysis Sessions are Associated with Increased Mortality, Independent of Body Weight. Kidney Int. 2013;83(1):104–13. doi:10.1038/ki.2012.346
41. Yuliawati AN, Ratnasari PMD, Pratiwi IGAS. Hubungan Kepatuhan Pengobatan dengan Kualitas Hidup Pasien Gagal Ginjal Kronik Disertai Hipertensi dan Menjalani Hemodialisis. J Manag Pharm. 2022;12(1):28-39. doi:10.22146/jmpf.69974
Authors
Copyright (c) 2023 Agustina Nila Yuliawati, Pande Made Desy Ratnasari, Ni Luh Putu Satria Maharani

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.