Appropriateness and Cost of Prophylaxis Stress Ulcer for Inpatient in the Internal Medicine Department in a Government Hospital: A Cross-Sectional Study
Abstract
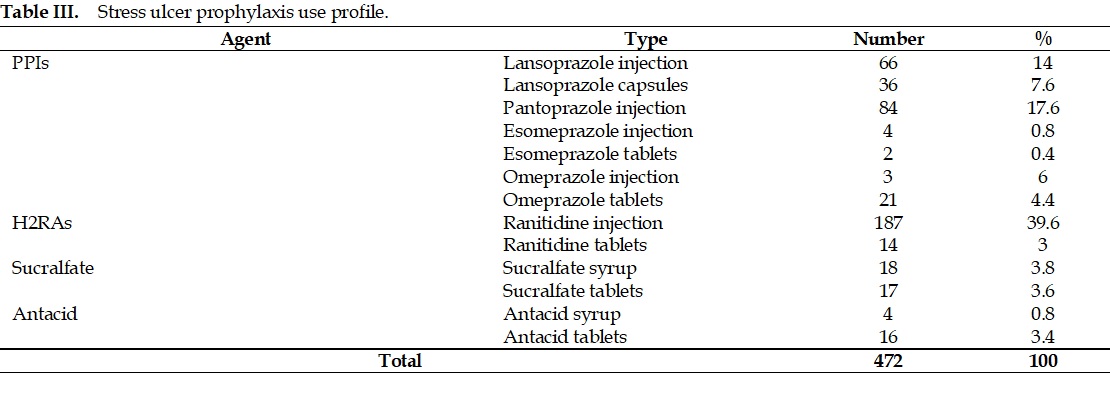
Guidelines from the American Society of Health-System Pharmacists (ASHP) 1999 prohibit acid-suppressing therapy for stress ulcer prophylaxis (SUP) in patients who are not critically ill. Stress ulcer prophylaxis is not recommended in non-ICU patients with <2 risk factors. Inappropriate use of SUP can increase costs for patients. This study aims to evaluate the use and the cost of SUP. This research was a non-experimental observational study with a cross-sectional approach. Data was collected retrospectively using the consecutive sampling method with a random sampling technique on the medical records of inpatients in the internal medicine ward of Sleman Regional Public Hospital from January to December 2020, totaling 340 samples. The results showed that proton pump inhibitors were the most widely used acid-suppressing drugs, with 45.8%. Furthermore, the histamine-2 receptor antagonist was 42.6%, the sucralfate group was 7.4%, and the antacid group was 4.2%. Of 340 patients, 57 (16.8%) were in the proper indication based on the guidelines, and 283 (83.2%) were under the wrong indication for SUP. They were using SUP with the proper indication so that the therapy could save treatment costs by Rp. 19,933,582. There was a high prevalence of inappropriate SUP prescriptions among inpatients in the internal medicine department; if these drugs were given with the appropriate indications, they could save more on the prophylaxis cost. Clinician pharmacists should develop an effective intervention strategy to reduce inappropriate SUP drugs.
Full text article
References
2. Choi YJ, Sim J, Jung YT, Shin S. Impact of a multidisciplinary quality improvement initiative to reduce inappropriate usage of stress ulcer prophylaxis in hospitalized patients. Br J Clin Pharmacol. 2020;86(5):903–12. DOI: 10.1111/bcp.14197; PMCID: PMC7163370; PMID: 31840265
3. Armstrong TA, Coursin DB, Devlin J, Duke JS, Fish D, Gonzales ER, et al. ASHP Therapeutic Guidelines on Stress Ulcer Prophylaxis. ASHP Commission on Therapeutics and approved by the ASHP Board of Directors on November 14, 1998. Am J Health Syst Pharm. 1999;56(4):347–79. DOI: 10.1093/ajhp/56.4.347; PMID: 10690219
4. Herzig SJ, Rothberg MB, Feinbloom DB, Howell MD, Ho KKL, Ngo LH, et al. Risk factors for nosocomial gastrointestinal bleeding and use of acid-suppressive medication in non-critically ill patients. J Gen Intern Med. 2013;28(5):683–90. DOI: 10.1007/s11606-012-2296-x; PMCID: PMC3631055; PMID: 23292499
5. Hong MT, Monye LC, Seifert CF. Acid Suppressive Therapy for Stress Ulcer Prophylaxis in Noncritically Ill Patients. Ann Pharmacother. 2015;49(9):1004–8. DOI: 10.1177/1060028015592014; PMID: 26139638
6. Jaynes M, Kumar AB. The risks of long-term use of proton pump inhibitors: a critical review. Ther Adv Drug Saf. 2018;10:2042098618809927. DOI: 10.1177/2042098618809927; PMCID: PMC6463334; PMID: 31019676
7. Buendgens L, Koch A, Tacke F. Prevention of stress-related ulcer bleeding at the intensive care unit: Risks and benefits of stress ulcer prophylaxis. World J Crit Care Med. 2016;5(1):57-64. DOI: 10.5492/wjccm.v5.i1.57; PMCID: PMC4733456; PMID: 26855894
8. Barletta JF, Sclar DA. Proton pump inhibitors increase the risk for hospital-acquired Clostridium difficile infection in critically ill patients. Crit Care. 2014;18(6):714. DOI: 10.1186/s13054-014-0714-7; PMCID: PMC4293826; PMID: 25540023
9. Farsaei S, Ghorbani S, Adibi P. Variables Associated with Adherence to Stress Ulcer Prophylaxis in Patients Admitted to the General Hospital Wards: A Prospective Study. Adv Pharm Bull. 2017;7(1):73-80. DOI: 10.15171/apb.2017.009; PMCID: PMC5426736; PMID: 28507939
10. Parsons C, Chung-Esaki H, Berte N. Medication Monitoring: Stress Ulcer Prophylaxis Clinical Guidelines. Stanford (CA): Stanford Hospital and Clinics, Pharmacy Department Policies and Procedures; 2015. Available from: https://med.stanford.edu/content/dam/sm/bugsanddrugs/documents/clinicalpathways/SHC-Stress-Ulcer-Prophylaxis-Protocol.pdf
11. Horsa BA, Ayele Y, Ayalew MB. Assessment of pharmacologic prophylaxis use against stress ulcer in the medical wards of University of Gondar Hospital. SAGE Open Med. 2019;7:205031211982740. DOI: 10.1177/2050312119827409; PMCID: PMC6360640; PMID: 30746144
12. Kementerian Kesehatan Republik Indonesia. Laporan Hasil Riset Kesehatan Dasar (Riskesdas) 2013. Jakarta: Badan Penelitian dan Pengembangan Kesehatan, Kementerian Kesehatan Republik Indonesia; 2013.
13. Nehlig A. Effects of Coffee on the Gastro-Intestinal Tract: A Narrative Review and Literature Update. Nutrients. 2022;14(2):399. DOI: 10.3390/nu14020399; PMCID: PMC8778943; PMID: 35057580
14. Ilham MI, Haniarti, Usman. Hubungan Pola Konsumsi Kopi Terhadap Kejadian Gastritis Pada Mahasiswa Muhammadiyah Parepare. J Ilmu Manusia Kesehatan. 2013;53(9):1689–99. DOI: 10.31850/makes.v2i3.189
15. Lei T, Shi M, Lei X, Xu G, Huang Y, Lei T, et al. Upper gastrointestinal bleeding in elderly patients: An analysis of 210 cases. World Chinese J Dig. 20(32):3164. DOI: 10.11569/wcjd.v20.i32.3164
16. Issa IA, Soubra O, Nakkash H, Soubra L. Variables Associated with Stress Ulcer Prophylaxis Misuse: A Retrospective Analysis. Dig Dis Sci. 2012;57(10):2633–41. DOI: 10.1007/s10620-012-2104-9; PMID: 22427129
17. Huang WC, Lee IK, Chen YC, Tsai CY, Liu JW. Characteristics and predictors for gastrointestinal hemorrhage among adult patients with dengue virus infection: Emphasizing the impact of existing comorbid disease(s). PLoS One. 2018;13(2):e0192919. DOI: 10.1371/journal.pone.0192919; PMCID: PMC5819790; PMID: 29462169
18. Defryantho R, Amalia L, Rizal A, Gunadharma S, Aminah S, Lailiyya N. Hubungan Perdarahan Gastrointestinal dengan Luaran Pasien Stroke Iskemik Akut. Neurona. 2019;36(2):79-86. DOI: 10.52386/neurona.v36i2.58
19. Octavia M, Ikawati Z, Andayani TM. Kajian Efektivitas Lansoprazol dan Pantoprazol sebagai Profilaksis Stress Ulcers di Intensive Care Unit (ICU). MPI Media Pharm Indones. 2019;2(3):165–72. DOI: 10.24123/mpi.v2i3.1568
20. Sheikh-Taha M, Alaeddine S, Nassif J. Use of acid suppressive therapy in hospitalized non-critically ill patients. World J Gastrointest Pharmacol Ther. 2012;3(6):93-6. DOI: 10.4292/wjgpt.v3.i6.93; PMCID: PMC3596518; PMID: 23494814
21. Abukhalil AD, Ali O, Saad A, Falana H, Al-Shami N, Naseef HA, et al. Evaluation of Proton Pump Inhibitors Prescribing Among Hospitalized Patients: A Cross-Sectional Study. Int J Gen Med. 2023;16:141–50. DOI: 10.2147/ijgm.s396202; PMCID: PMC9843499; PMID: 36659914
22. Korayem GB, Alkanhal R, Almass R, Alkhunaizan S, Alharthi G, Bin Sheraim N, et al. Patients, Prescribers, and Institutional Factors Associated with Inappropriate Use of Acid Suppressive Therapy in Medical Wards: An Experience of a Single-Center in Saudi Arabia. Int J Gen Med. 2021; 14:5079–89. DOI: 10.2147/ijgm.s328914; PMCID: PMC8416456; PMID: 34511990
23. Mohamad MS, Shamsuddin N, Tan KM. Appropriateness of stress ulcer prophylaxis among older adults admitted to general medical wards in a university hospital. Eur Geriatr Med. 2015;6(2):119–23. DOI: 10.1016/j.eurger.2014.11.004
24. Alshamsi F, Belley-Cote E, Cook D, Almenawer SA, Alqahtani Z, Perri D, et al. Efficacy and safety of proton pump inhibitors for stress ulcer prophylaxis in critically ill patients: a systematic review and meta-analysis of randomized trials. Crit Care. 2016;20(1):120. DOI: 10.1186/s13054-016-1305-6; PMCID: PMC4855320; PMID: 27142116
25. Malhis A, Alghamdi T, Alfandi R, Issa Z, Alanazi H, Alfintoukh H, et al. Appropriateness of acid-suppressing agents for stress ulcer prophylaxis in non-intensive care unit setting in Saudi Arabia. J Pharm Bioallied Sci. 2019;11(1):96-101. DOI: 10.4103/jpbs.jpbs_173_18; PMCID: PMC6394160; PMID: 30906145
26. Li H, Li N, Jia X, Zhai Y, Xue X, Qiao Y. Appropriateness and Associated Factors of Stress Ulcer Prophylaxis for Surgical Inpatients of Orthopedics Department in a Tertiary Hospital: A Cross-Sectional Study. Front Pharmacol. 2022;13:881063. DOI: 10.3389/fphar.2022.881063; PMCID: PMC9203048; PMID: 35721126
27. Pratiwi H, Maharani L, Mustikaningtias I. Cost Saving of Stress Ulcer Prophylaxis Used in Non-Intensive Care Unit (ICU) Inpatients. MPI Media Pharm Indones. 2020;3(1):37–43. DOI: 10.24123/mpi.v3i1.2323
28. Xin C, Dong Z, Lin M, Li GH. The impact of pharmaceutical interventions on the rational use of proton pump inhibitors in a Chinese hospital. Patient Prefer Adherence. 2017;12:21–6. DOI: 10.2147/ppa.s150388; PMCID: PMC5749561; PMID: 29343945
Authors
Copyright (c) 2024 Mega Octavia, Nurul Maziyyah, Rima Nurul Fauziyah

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.