Effects of Switching Dose, Dose Variation, and Warfarin Interaction on the Incidence of Stroke Recurrence in Stroke Patients with Atrial Fibrillation
Abstract
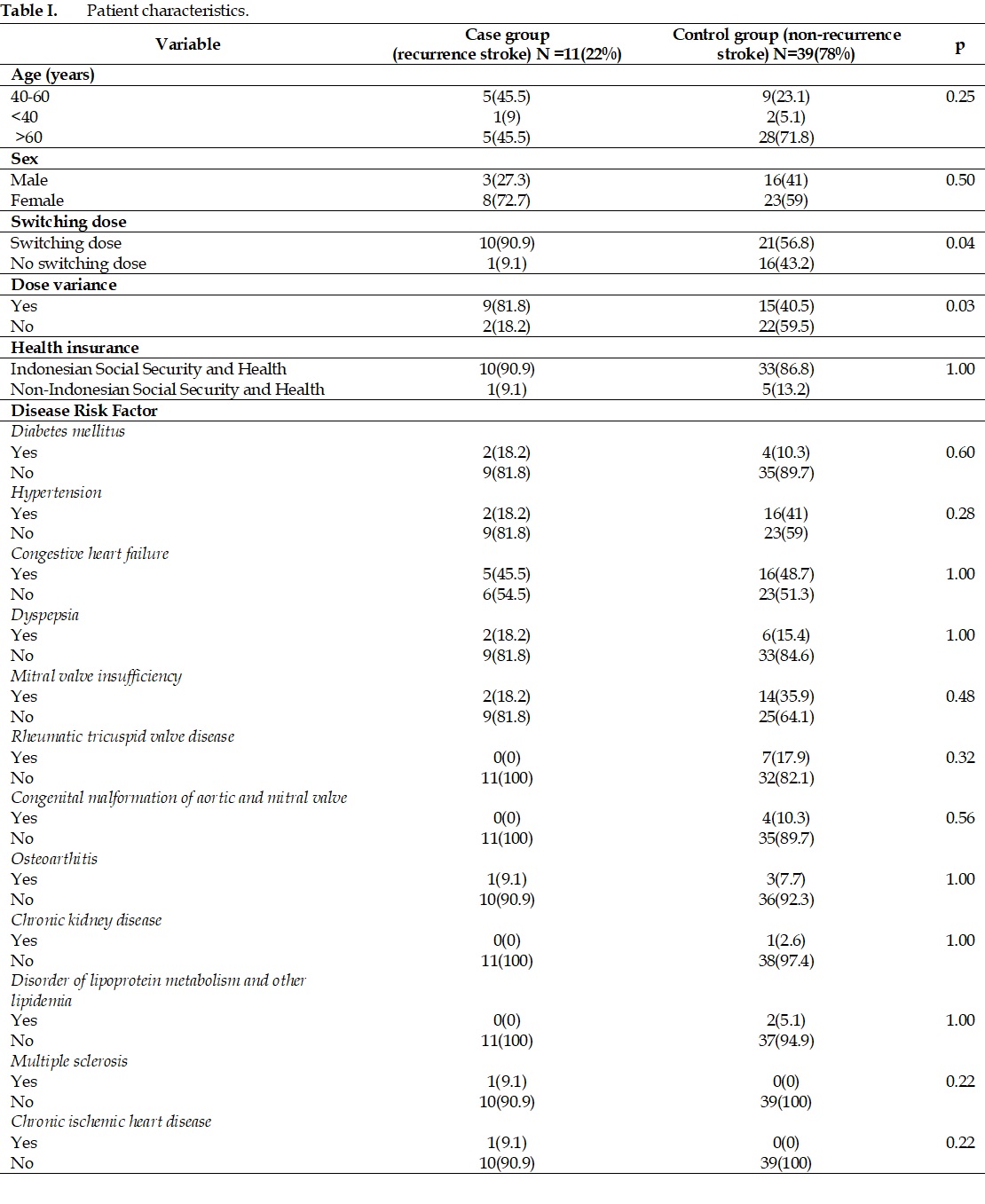
Atrial fibrillation (AF) significantly increases the risk of stroke, necessitating anticoagulation therapy. Warfarin, a commonly prescribed anticoagulant regimen, requires careful monitoring to ensure patient safety. This study aimed to assess the impact of dose switching, dose variation, and potential interactions with warfarin on the incidence of stroke recurrence in stroke patients with AF. The study retrospectively analyzed the treatment records of stroke patients with AF in outpatient settings over one year. The subjects comprised 314 patients who received warfarin prescriptions at two Indonesian Hospitals from January 1, 2015, to December 31, 2019. Out of these patients, 50 had recorded data regarding dose adjustments, variations, and interactions. They were divided into two groups: a case group (n=11) with stroke recurrence and a control group (n=39) without recurrence. Statistical analysis, including chi-square tests and odds ratio calculations, revealed that both warfarin dose switching (OR=7.6) and dose variation (OR=6.6) significantly influenced the incidence of stroke recurrence. It implies that inconsistencies or alterations in warfarin dosing substantially elevate the likelihood of experiencing another stroke, potentially due to inadequate anticoagulation leading to clot formation. Interestingly, the analysis of drug interactions did not significantly impact stroke recurrence. In summary, the recurrence of stroke in patients with AF is notably influenced by warfarin dose adjustments and variations rather than drug interactions. This study highlights the critical importance of precise dosing strategies and vigilant monitoring to enhance the efficacy of anticoagulant therapy in this high-risk population.
Full text article
References
2. Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022;17(1):18–29. DOI: 10.1177/17474930211065917; PMID: 34986727
3. Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2017;115(5):e69-171. DOI: 10.1161/circulationaha.106.179918; PMID: 17194875
4. Damayanti A, Amalia L, Sudjud RW. Characteristics of Cardioembolic Stroke Patient in Neurologic Ward Dr. Hasan Sadikin General Hospital Bandung. J Med Health. 2018;2(1):630–6. DOI: 10.28932/jmh.v2i1.740
5. Camm AJ, Lip GYH, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–47. DOI: 10.1093/eurheartj/ehs253; PMID: 22922413
6. Zhao Y, Zou C, Wang C, Zhang Y, Wang S. Long-term outcomes after stroke in elderly patients with atrial fibrillation: a hospital-based follow-up study in China. Front Aging Neurosci. 2016;8:56. DOI: 10.3389/fnagi.2016.00056; PMCID: PMC4809894; PMID: 27065856
7. Indonesian Heart Association. Pedoman Tata Laksana Fibrilasi Atrium Nonvalvular. 2nd edition. In: Munawar M, Yuniadi Y, editors. Jakarta: Indonesian Heart Association; 2018.
8. Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G. Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e44S-e88S. DOI: 10.1378/chest.11-2292; PMCID: PMC3278051; PMID: 22315269
9. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 130(23):199–267. DOI: 10.1161/cir.0000000000000040; PMID: 24682348
10. Di Minno A, Frigerio B, Spadarella G, Ravani A, Sansaro D, Amato M, et al. Old and new oral anticoagulants: Food, herbal medicines and drug interactions. Blood Rev. 2017;31(4):193-203. DOI: 10.1016/j.blre.2017.02.001; PMID: 28196633
11. Kuruvilla M, Gurk-Turner C. A review of warfarin dosing and monitoring. Proc (Bayl Univ Med Cent). 2001;14(3):305-6. DOI: 10.1080/08998280.2001.11927781; PMCID: PMC1305837; PMID: 16369639
12. Teklay G, Shiferaw N, Legesse B, Bekele ML. Drug-drug interactions and risk of bleeding among inpatients on warfarin therapy: a prospective observational study. Thromb J. 2014;12:20. DOI: 10.1186/1477-9560-12-20; PMCID: PMC4171718; PMID: 25249791
13. Rikala M, Hauta-Aho M, Helin-Salmivaara A, Lassila R, Korhonen MJ, Huupponen R. Co-Prescribing of Potentially Interacting Drugs during Warfarin Therapy - A Population-Based Register Study. Basic Clin Pharmacol Toxicol. 2015;117(2):126–32. DOI: 10.1111/bcpt.12373; PMID: 25537751
14. Nilamsari WP, Yusuf M, Pertiwi DA, Dery A, Budi S, Zulkarnaen B. Study of co-prescription of drugs potentially interacting with warfarin in indonesian ambulatory patients. Res J Pharm Technol. 2020;13(8):3833–6. DOI: 10.5958/0974-360X.2020.00678.2
15. Ding M, Ebeling M, Ziegler L, Wennberg A, Modig K. Time trends in atrial fibrillation-related stroke during 2001-2020 in Sweden: a nationwide, observational study. Lancet Reg Health Eur. 2023;28:100596. DOI: 10.1016/j.lanepe.2023.100596; PMCID: PMC10173271; PMID: 37180742
16. Lu Y, Shen D, Pietsch M, Nagar C, Fadli Z, Huang H, et al. A novel algorithm for analyzing drug-drug interactions from MEDLINE literature. Sci Rep. 2015;5:1–10. DOI: 10.1038/srep17357; PMCID: PMC4661569; PMID: 26612138
17. Oxford University Hospitals. Oxford Haemophilia and Thrombosis Centre Protocols for Outpatient Oral Anticoagulation with Vitamin K Antagonists. Oxford: Oxford University Hospitals; 2017.
18. Yancy CW, Bozkurt MJB, Butler J, Casey Jr DE, Colvin MM, Drazner MH, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137-61. DOI: 10.1161/cir.0000000000000509; PMID: 28455343
19. Alhumaidi RM, Bamagous GA, Alsanosi SM, Alqashqari HS, Qadhi RS, Alhindi YZ, et al. Risk of Polypharmacy and Its Outcome in Terms of Drug Interaction in an Elderly Population: A Retrospective Cross-Sectional Study. J Clin Med. 2023;12(12):3960. DOI: 10.3390/jcm12123960; PMCID: PMC10299180; PMID: 37373654
20. Hamadouk RM, Alshareif EM, Hamad HM, Yousef BA. The Prevalence and Severity of Potential Drug-Drug Interactions in Internal Medicine Ward at Soba Teaching Hospital. Drug Healthc Patient Saf. 2023;15:149-57. DOI: 10.2147/dhps.s436458; PMCID: PMC10625782; PMID: 37933264
21. Manolis AJ, Poulimenos LE. Prevention of stroke by antithrombotic therapy in patients with atrial fibrillation. J Atr Fibrillation. 2013;5(5):84–92. DOI: 10.4022/jafib.732; PMCID: PMC5153105; PMID: 28496810
22. Hindsholm MF, Damgaard D, Gurol ME, Gaist D, Simonsen CZ. Management and Prognosis of Acute Stroke in Atrial Fibrillation. J Clin Med. 2023;12(17):5752. DOI: 10.3390/jcm12175752; PMCID: PMC10489015; PMID: 37685819
23. Björck S, Palaszewski B, Friberg L, Bergfeldt L. Atrial fibrillation, stroke risk, and warfarin therapy revisited: A population-based study. Stroke. 2013;44(11):3103–8. DOI: 10.1161/strokeaha.113.002329; PMID: 23982711
24. Katsanos AH, Kamel H, Healey JS, Hart RG. Stroke Prevention in Atrial Fibrillation Looking Forward. Circulation. 2020;142(24):2371–88. DOI: 10.1161/circulationaha.120.049768; PMID: 33315494
25. Vega AJ, Smith C, Matejowsky HG, Thornhill KJ, Borne GE, Mosieri CN, et al. Warfarin and Antibiotics: Drug Interactions and Clinical Considerations. Life. 2023;13(8):1661. DOI: 10.3390/life13081661
26. Acar T, Aras YG, Gül SS, Acar BA. Effective INR level may be delayed in secondary prevention of stroke due to atrial fibrillation with warfarin in the patients with diabetes mellitus. Noro Psikiyatr Ars. 2019;56(4):273–6. DOI: 10.29399/npa.23395; PMCID: PMC6927077; PMID: 31903036
27. Shikdar S, Vashisht R, Bhattacharya PT. International normalized ratio (INR). In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2018. PMID: 29939529
28. Sánchez-Acosta K, Galeano L, Villarreal D, Montoya A, Bayona H. Recurrent stroke due to atrial fibrillation: perspectives about an unsolved problem. Rev Colomb Cardiol. 2023;30(3):185–92. DOI: 10.24875/RCCARE.M22000023
29. Yamashita T, Akao M, Atarashi H, Ikeda T, Koretsune Y, Okumura K, et al. Effect of Polypharmacy on Clinical Outcomes in Elderly Patients With Non-Valvular Atrial Fibrillation - A Sub-Analysis of the ANAFIE Registry. Circ J. 2022;87(1):6–16. DOI: 10.1253/circj.cj-22-0170; PMID: 35858804
30. Aleksic DZ, Jankovic SM, Mlosavljevic MN, Toncev GL, Miletic Drakulic SD, Stefanovic SM. Potential drug-drug interactions in acute ischemic stroke patients at the Neurological Intensive Care Unit. Open Med. 2019;14(1):813–26. DOI: 10.1515/med-2019-0093; PMCID: PMC6843487; PMID: 31737786
31. Hosseini S, Zabihi A, Jafarian Amiri S, Bijani A. Polypharmacy among the elderly. J Midlife Health. 2018;9(2):97–103. DOI: 10.4103/jmh.jmh_87_17; PMCID: PMC6006800; PMID: 29962809
Authors
Copyright (c) 2024 Lailla Affianti Fauzi, Erna Kristin, Rizaldy Taslim Pinzon, Bernadeta Margareta Wara Kushartanti, Novita Intan Arovah

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.