Antihypertension Profile During Pregnancy at a Private Hospital in Surabaya
Abstract
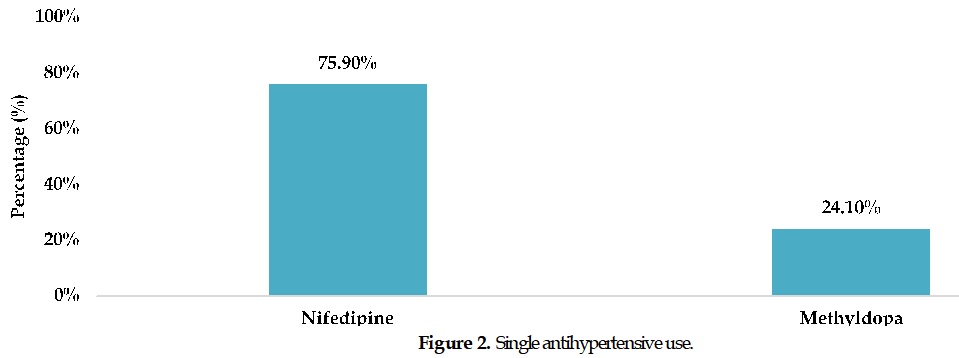
Hypertension during pregnancy, a significant obstetric complication, can lead to severe consequences such as preeclampsia. This study aimed to determine the pattern of antihypertensive medication use, including drug type, route of administration, dosage, and frequency, as well as investigate the relationship between clinical data, including blood pressure and proteinuria, and the use of single or combination antihypertensive therapy in pregnant women with hypertension. A retrospective observational study was conducted on 108 pregnant women with hypertension admitted to the inpatient unit of a private hospital in Surabaya, Indonesia. Data on patient demographics, comorbidities, antihypertensive medications, blood pressure, and proteinuria levels were collected and analyzed. The majority (79.65%) of patients were aged between 20 and 35 years. Common comorbidities included obesity (62.50%), pre-existing hypertension (18.75%), and a history of preeclampsia in previous pregnancies (6.25%). Nifedipine (73.26%) was the most frequently used single antihypertensive medication, followed by methyldopa (23.26%). Combination therapy, primarily nifedipine and methyldopa (92.31%), was commonly employed. Most patients (97.35%) achieved blood pressure control, and 47.79% showed improvement in proteinuria levels. Nifedipine and the combination of nifedipine and methyldopa were the most frequently used antihypertensive medications in this cohort. Most patients achieved blood pressure control, indicating effective management of hypertension during pregnancy. Further studies are warranted to investigate the long-term outcomes and optimize antihypertensive therapy strategies in this population.
Full text article
References
2. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension, 75(6):1334-57. DOI: 10.1161/hypertensionaha.120.15026; PMID: 32370572
3. Bajpai D, Popa C, Verma P, Dumanski S, Shah S. Evaluation and Management of Hypertensive Disorders of Pregnancy. Kidney360. 2023;4(10):1512-25. DOI: 10.34067/kid.0000000000000228; PMCID: PMC10617800; PMID: 37526641
4. Ekwuazi EK, Chigbu CO, Ngene NC. Reducing maternal mortality in low- and middle-income countries. Case Rep Womens Health. 2023;39:e00542. DOI: 10.1016/j.crwh.2023.e00542; PMCID: PMC10636262; PMID: 37954228
5. Suparji S, Nugroho HSW, Sunarto S, Prayogi AS. High maternal mortality rate in Indonesia: a challenge to be addressed immediately. PAMJ-One Health. 2024;14:13. DOI: 10.11604/pamj-oh.2024.14.13.44464
6. Febriyanto EC, Indawati R, Mahmudah, Ama F, Ashari FY. Modeling of Maternal Mortality (MMR) in East Java 2017-2019 Using Panel Regression Approach. J Biometrika Kependudukan. 2023;12(2):177-85. DOI: 10.20473/jbk.v12i2.2023.177-185
7. Sulistyono A, Joewono HT, Yustinasari, Aditiawarman. Maternal mortality from eclampsia at tertiary referral hospital, Surabaya, Indonesia. Eurasia J Biosci. 2020;14:1709-13.
8. Ernawaty E, Sri D. Health Expenditure Analysis in Patients with Pregnancy-Labor Complications in Surabaya. Indones J Health Adm. 2022;10(1):3-13. DOI: 10.20473/jaki.v10i1.2022.3-13
9. Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cífková R, Dominiczak AF, et al. Hypertension. Nat Rev Dis Primers. 2018;4:18014. DOI: 10.1038/nrdp.2018.14; PMCID: PMC6477925; PMID: 29565029
10. Awaludin A, Rahayu C, Daud NAA, Zakiyah N. Antihypertensive Medications for Severe Hypertension in Pregnancy: A Systematic Review and Meta-Analysis. Healthcare. 2022;10(2):325. DOI: 10.3390/healthcare10020325; PMCID: PMC8872490; PMID: 35206939
11. Donel S, Novri DA, Hamidy Y, Savira M. Effectiveness of nifedipine, labetalol, and hydralazine as emergency antihypertension in severe preeclampsia: a randomized control trial. F1000Res. 2023;11:1287. DOI: 10.12688/f1000research.125944.2; PMCID: PMC10238817; PMID: 37273965
12. Hazra PK, Mehta A, Desai B, Pandey U, Mehta KD, Bajpai S, et al. Long-acting nifedipine in the management of essential hypertension: a review for cardiologists. Am J Cardiovasc Dis. 2024;14(6):396-413. DOI: 10.62347/rpmz6407; PMCID: PMC11744219; PMID: 39839565
13. Snider ME, Nuzum DS, Veverka A. Long-acting nifedipine in the management of the hypertensive patient. Vasc Health Risk Manag. 2008;4(6):1249-57. DOI: 10.2147/vhrm.s3661; PMCID: PMC2663456; PMID: 19337538
14. Easterling T, Mundle S, Bracken H, Parvekar S, Mool S, Magee LA, et al. Oral antihypertensive regimens (nifedipine retard, labetalol, and methyldopa) for management of severe hypertension in pregnancy: an open-label, randomised controlled trial. Lancet. 2019;394(10203):1011-21. DOI: 10.1016/S0140-6736(19)31282-6; PMCID: PMC6857437; PMID: 31378394
15. Gradman AH, Basile JN, Carter BL, Bakris GL. Combination Therapy in Hypertension. J Clin Hypertens. 2010;13(3):146-54. DOI: 10.1111/j.1751-7176.2010.00397.x; PMCID: PMC8673364; PMID: 21366845
16. Brown CM, Garovic VD. Drug Treatment of Hypertension in Pregnancy. Drugs. 2014;74(3):283-96. DOI: 10.1007/s40265-014-0187-7; PMCID: PMC4558097; PMID: 24554373
17. Campbell S, Greenwood M, Prior S, Shearer T, Walkem K, Young S, et al. Purposive sampling: complex or simple? Research case examples. J Res Nurs. 2020;25(8):652-61. DOI: 10.1177/1744987120927206; PMCID: PMC7932468; PMID: 34394687
18. Chang KJ, Seow KM, Chen KH. Preeclampsia: Recent Advances in Predicting, Preventing, and Managing the Maternal and Fetal Life-Threatening Condition. Int J Environ Res Public Health. 2023;20(4):2994. DOI: 10.3390/ijerph20042994; PMCID: PMC9962022; PMID: 36833689
19. Karrar SA, Martingano DJ, Hong PL. Preeclampsia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025. PMID: 34033373
20. Ernawati, Aditiwarman, Rifdah SN, Sulistyono A. Antihypertensive Choices during Pregnancy in Limited Setting. Pharmacogn J. 2023;15(2):315-8. DOI: 10.5530/pj.2023.15.46
21. Stason WB, Schmid CH, Niedzwiecki D, Whiting GW, Caubet JF, Luo D, et al. Safety of nifedipine in patients with hypertension: a meta-analysis. Hypertension. 1997;30(1 Pt 1):7-14. DOI: 10.1161/01.hyp.30.1.7; PMID: 9231814
22. Cífková R. Hypertension in Pregnancy: A Diagnostic and Therapeutic Overview. High Blood Press Cardiovasc Prev. 2023;30(4):289-303. DOI: 10.1007/s40292-023-00582-5; PMCID: PMC10403432; PMID: 37308715
23. Sarafidis PA, Khosla N, Bakris GL. Antihypertensive therapy in the presence of proteinuria. Am J Kidney Dis. 2007;49(1):12-26. DOI: 10.1053/j.ajkd.2006.10.014; PMID: 17185142
24. Marlina Y, Santoso H, Sirait A. Faktor-Faktor Yang Berhubungan Dengan Hipertensi Pada Ibu Hamil di Wilayah Kerja Puskesmas Padang Panyang Kecamatan Kuala Pesisir Kabupaten Nagan Raya. J Healthc Technol Med. 2022; 7(2):1512-25. DOI: 10.33143/jhtm.v7i2.1734
25. Dewie A, Pont AV, Purwanti A. Hubungan Umur Kehamilan dan Obesitas Ibu Hamil dengan Kejadian Preeklampsia di Wilayah Kerja Puskesmas Kampung Baru Kota Luwuk. Promotif J Kesehatan Masyarakat. 2020;10(1):21–7. DOI: 10.56338/pjkm.v10i1.616
26. Kepley JM, Bates K, Mohiuddin SS. Physiology, Maternal Changes. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025. PMID: 30969588
27. Bardja S. Faktor Risiko Kejadian Preeklampsia Berat/Eklampsia pada Ibu Hamil. EMBRIO J Kebidanan. 2020;12(1):18–30. DOI: 10.36456/embrio.v12i1.2351
28. Silvana R, Ramayanti I, Kurniawan, Ramadhina AD. Hubungan Antara Usia Ibu, Status Gravida, dan Riwayat Hipertensi dengan Terjadinya Preeklampsia. ULIL ALBAB J Ilmiah Multidisiplin. 2023;2(4):1370–5.
29. Perkumpulan Obstetri dan Ginekologi Indonesia. Pedoman Nasional Pelayanan Kedokteran Diagnosis dan Tata Laksana Preeklamsia. Jakarta: Perkumpulan Obstetri dan Ginekologi Indonesia; 2016.
30. Hidayati SF, Andarini YD, Marfu’ah N. Evaluasi Penggunaan Obat Antihipertensi pada Pasien Ibu Hamil di Instalasi Rawat Inap RSIA Muslimat Jombang Tahun 2018. Pharmasipha Pharm J Islam Pharm. 2020;4(2):66-73. DOI: 10.21111/pharmasipha.v4i2.4959
31. Kernaghan D, Duncan AC, McKay GA. Hypertension in pregnancy: a review of therapeutic options. Obstet Med. 2012;5(2):44-9. DOI: 10.1258/om.2011.110061; PMCID: PMC4989617; PMID: 27579135
32. Lee H, Park MS, Kang MK, Song TJ. Association between Proteinuria Status and Risk of Hypertension: A Nationwide Population-Based Cohort Study. J Pers Med. 2023;13(9):1414. DOI: 10.3390/jpm13091414; PMCID: PMC10533010; PMID: 37763181
Authors
Copyright (c) 2025 Oktaviany Irma Wiputri, Iftakhur Rahma, Karima Samlan

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.