The Effect of Directly Observed Treatment Strategy on Cost Utility of Pulmonary Tuberculosis Patients at Banten Regional Public Hospital
Abstract
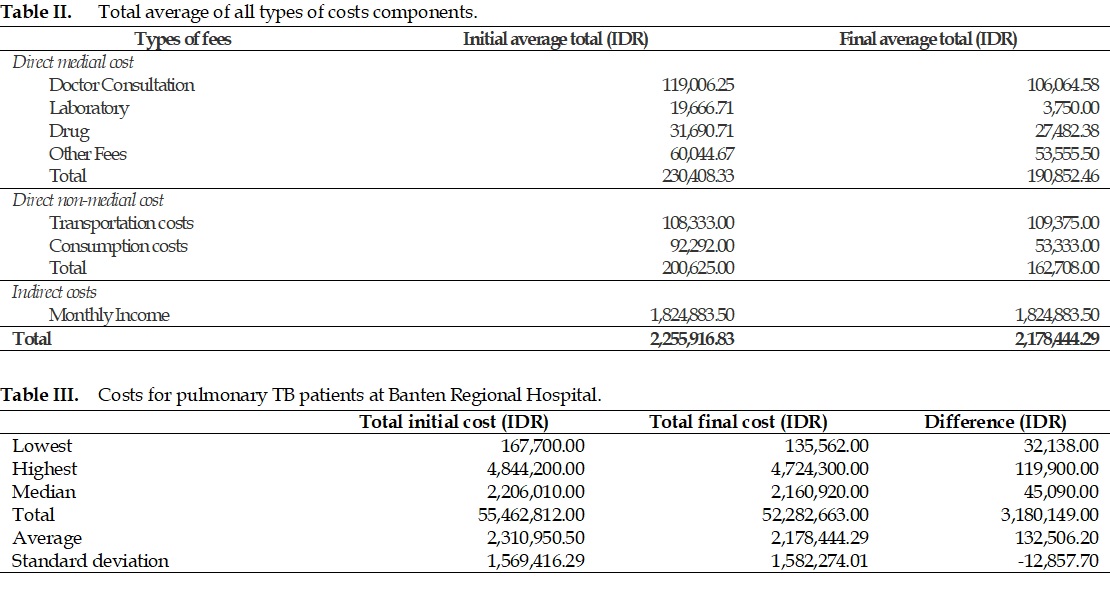
Pulmonary tuberculosis (TB) is one of the communicable diseases with high prevalence in some provinces in Indonesia, including the Province of Banten. Considering its high prevalence and the high cost of treatment resulting from multiple treatment components, research on the analysis of treatment costs of TB is very important. This study aimed to determine the effect of implementing the directly observed treatment (DOT) strategy on the cost-utility of pulmonary TB patients. The study was conducted at Banten Regional General Hospital using the perspective of the health provider and patients by involving 24 TB patients. Treatment cost was calculated by including direct medical costs, direct non-medical costs, and indirect costs, and then categorized into initial and final cost-utility. The average cost-effectiveness ratio (ACER) was then calculated by setting the patient's quality of life as the clinical outcome in this study. This study found that the average value of the average cost-utility ratio (ACUR) for the initial cost-utility and the final cost-utility were IDR 2,682,343.53 and IDR 2,402,153.15, respectively, and the difference was statistically significant (p=0.006). It indicates that the DOT strategy can potentially improve the utility costs of the treatment of TB patients at Banten Regional Hospital.
Full text article
References
2. Goletti D, Pisapia R, Fusco FM, Aiello A, Van Crevel R. Epidemiology, pathogenesis, clinical presentation and management of TB in patients with HIV and diabetes. Int J Tuberc Lung Dis. 2023;27(4):284-90. DOI: 10.5588/ijtld.22.0685; PMCID: PMC10094052; PMID: 37035976
3. UNICEF Indonesia. 2022. Desk Review: Pediatric Tuberculosis with a Focus on Indonesia. Jakarta: UNICEF Indonesia. Available from: https://www.unicef.org/indonesia/media/14436/file/Desk%20Review:%20Pediatric%20Tuberculosis%20with%20a%20Focus%20on%20Indonesia.pdf
4. Boadu AA, Yeboah-Manu M, Osei-Wusu S, Yeboah-Manu D. Tuberculosis and diabetes mellitus: The complexity of the comorbid interactions. Int J Infect Dis. 2024;146:107140. DOI: 10.1016/j.ijid.2024.107140; PMID: 38885832
5. Yusransyah Y, Stiani SN, Ismiyati R, Maharani S, Sumarlin US, Ernawati EE. Upaya Peningkatan Kesadaran Masyarakat Kabupaten Pandeglang Dalam Pencegahan Penyakit Diabetes Dan Tuberculosis. J Abdi Masyarakat Kita. 2023;3(2):95–103. DOI: 10.33759/asta.v3i2.419
6. Out AA. Is the directly observed therapy short course (DOTS) an effective strategy for tuberculosis control in a developing country? Asian Pac J Trop Dis. 2013;3(3):227-31. DOI: https://doi.org/10.1016/S2222-1808(13)60045-6; PMCID: PMC4027301
7. Yusransyah Y, Annintan R, Chairani F, Udin B. Correlation of Medication Adherence with the Characteristics and Quality of Life of Tuberculosis Patients in Dr. Dradjat Prawiranegara Hospital. Med Sains J Ilmiah Kefarmasian. 2023;8(4):1557–68. DOI: 10.37874/ms.v8i4.1005
8. Yasobant S, Khatib MN, Syed ZQ, Gaidhane AM, Shah H, Narkhede K, et al. Health-Related Quality of Life (HRQoL) of Patients with Tuberculosis: A Review. Infect Dis Rep. 2022;14(4):509-24. DOI: 10.3390/idr14040055; PMCID: PMC9326555; PMID: 35893474
9. Ita W, Yusran S, Sety LOM. Gambaran Kualitas Hidup Penderita TB Paru di Wilayah Kerja Puskesmas Perumnas Kota Kendari Tahun 2019. Endemis J. 2020;1(1):27–32. DOI: 10.37887/ej.v1i1.11457
10. Alfauzan, Lucya V. Gambaran Kualitas Hidup Pada Penderita Tuberkulosis di Asia: Literature Review. J Ilmiah Keperawatan Sci J Nursing. 2021;7(3):65–70. DOI: 10.33023/jikep.v7i3.810
11. Burki TK. The global cost of tuberculosis. Lancet Respir Med. 2018;6(1):13. DOI: 10.1016/s2213-2600(17)30468-x; PMID: 29239796
12. Ministry of Health of the Republic of Indonesia. The Republic of Indonesia Joint External Monitoring Mission for Tuberculosis. Jakarta: Ministry of Health of the Republic of Indonesia; 2020.
13. Saragih S, Hafidz F, Nugroho A, Hatt L, C’Connel M, Caroline A, et al. Estimating the budget impact of a Tuberculosis strategic purchasing pilot study in Medan, Indonesia (2018-2019). Health Econ Rev. 2024;14(1):44. DOI: 10.1186/s13561-024-00518-2; PMCID: PMC11191151; PMID: 38904689
14. Purba FD, Hunfeld JAM, Iskandarsyah A, Fitriana TS, Sadarjoen SS, Ramos-Goñi JM, et al. The Indonesian EQ-5D-5L Value Set. Pharmacoeconomics. 2017;35(11):1153–65. DOI: 10.1007/s40273-017-0538-9; PMCID: PMC5656740; PMID: 28695543
15. Yusransyah, Halimah E, Suwantika AA. Measurement of the Quality of Life of Prolanis Hypertension Patients in Sixteen Primary Healthcare Centers in Pandeglang District, Banten Province, Indonesia, Using EQ-5D-5L Instrument. Patient Prefer Adherence. 2020;14:1103-9. DOI: 10.2147/ppa.s249085; PMCID: PMC7352006; PMID: 32753850
16. Saragih DE, Nasution A, Khairunnisa K. Cost of Illness Analysis and Quality of Life in Ischemic Stroke Patients in USU Medan Hospital. Asian J Pharm Res Dev. 2020;8(2):1-6. DOI: 10.22270/ajprd.v8i2.652
17. Sunarmi S, Kurniawaty K. Hubungan Karakteristik Pasien TB Paru dengan Kejadian Tuberkulosis. J ’Aisyiyah Medika. 2022;7(2):182–7. DOI: 10.36729/jam.v7i2.865
18. Dewanty LI, Haryanti T, Kurniawan TP. Kepatuhan Berobat Penderita TB Paru di Puskesmas Nguntoronadi I Kabupaten Wonogiri. J Kesehatan. 2016;9(1):39-43. DOI: 10.23917/jk.v9i1.3406
19. Moscibrodzki P, Enane LA, Hoddinott G, Brooks MB, Byron V, Furin J, et al. The Impact of Tuberculosis on the Well-Being of Adolescents and Young Adults. Pathogens. 2021;10(12):1591. DOI: 10.3390/pathogens10121591; PMCID: PMC8706072; PMID: 34959546
20. Caraux-Paz P, Diamantis S, de Wazières B, Gallien S. Tuberculosis in the Elderly. J Clin Med. 2021;10(24):5888. DOI: 10.3390/jcm10245888; PMCID: PMC8703289; PMID: 34945187
21. Widiati B, Majdi M. Analisis Faktor Umur, Tingkat Pendidikan, Pekerjaan, dan Tuberkulosis Paru di Wilayah Kerja Puskesmas Korleko, Kabupaten Lombok Timur. J Sanitasi Lingkungan. 2021;2(2):173–84.
22. Gao L, Luo B. Assessment of Factors Associated with Anti-Tubercular Treatment Compliance in Children: A Cross-Sectional Study. Glob Pediatr Health. 2024;11:2333794X231199360. DOI: 10.1177/2333794x231199360; PMCID: PMC10893831; PMID: 38405015
23. Gebreweld FH, Kifle MM, Gebremicheal FE, Simel LL, Gezae MM, Ghebreyesus SS, et al. Factors influencing adherence to tuberculosis treatment in Asmara, Eritrea: a qualitative study. J Health Popul Nutr. 2018;37(1):1. DOI: 10.1186/s41043-017-0132-y; PMCID: PMC5756387; PMID: 29304840
24. Fahdhienie F, Mudatsir, Abidin TF, Nurjannah. Risk factors of pulmonary tuberculosis in Indonesia: A case-control study in a high disease prevalence region. Narra J. 2024;4(2):e943. DOI: 10.52225/narra.v4i2.943; PMCID: PMC11391971; PMID: 39280301
25. Akadji HD, Boekoesoe L, Kadir L. Analisis Determinan Kejadian Tuberkulosis: Data Wilayah Kerja Puskesmas Tilango, Kabupaten Gorontalo. Health Inf J Penelitian. 2023;15(2):12–21.
26. Katiandagho D, Fione VR, Sambuaga J. Hubungan Merokok Dengan Kejadian TB Paru di Wilayah Kerja Puskesmas Tatelu Kecamatan Dimembe. In: Prosiding Seminar Nasional Tahun 2018. Manado: Poltekkes Kemenkes Manado; 2018. p. 582-93.
27. Nguyen HB, Vo LNQ, Forse RJ, Wiemers AMC, Huynh HB, Dong TTT, et al. Is convenience really king? Comparative evaluation of catastrophic costs due to tuberculosis in the public and private healthcare sectors of Viet Nam: a longitudinal patient cost study. Infect Dis Poverty. 2024;13(1):27. DOI: 10.1186/s40249-024-01196-2; PMCID: PMC10962209; PMID: 38528604
28. van Druten VP, Bartels EA, van de Mheen D, de Vries E, Kerckhoffs APM, Nahar-van-Venrooij LMW. Concepts of health in different contexts: a scoping review. BMC Health Serv Res. 2022;22:389. DOI: 10.1186/s12913-022-07702-2
29. Gautam S, Jain A, Chaudhary J, Gautam M, Gaur M, Grover S. Concept of mental health and mental well-being, it's determinants and coping strategies. Indian J Psychiatry. 2024;66(Suppl 2):S231-44. DOI: 10.4103/indianjpsychiatry.indianjpsychiatry_707_23; PMCID: PMC10911315; PMID: 38445271
30. Feng YS, Kohlmann T, Janssen MF, Buchholz I. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res. 2021;30:647-73. DOI: 10.1007/s11136-020-02688-y
31. Hadning I, Andayani TM, Endarti D, Triasih R. Health-Related Quality of Life Among Children with Pneumonia in Indonesia Using the EuroQoL Descriptive System Value Set for Indonesia. Value Health Res Issues. 2021;24:12-6. DOI: 10.1016/j.vhri.2020.05.010; PMID: 33465710
32. Tondok SB, Watu E, Wahyuni W. Validitas instrumen European Qualitiy of Life (EQ-5D-5L) Versi Indonesia untuk menilai kualitas hidup penderita tuberkulosis. Holistik J Kesehatan. 2021;15(2):267-73. DOI: 10.33024/hjk.v15i2.4759
33. Latif S, Sharyar M, Shafee I, Ali J, Mannan A, Deedar S, et al. Six Minute Walk Test in People with Tuberculosis Sequelae. Pakistan J Med Heal Sci. 2022;16(3):935–7. DOI: 10.53350/pjmhs22163935
34. Luies L, du Preez I. The Echo of Pulmonary Tuberculosis: Mechanisms of Clinical Symptoms and Other Disease-Induced Systemic Complications. Clin Microbiol Rev. 2020;33(4):e00036-20. DOI: 10.1128/cmr.00036-20; PMCID: PMC7331478; PMID: 32611585
35. Yudyarto HE, Taadi, Nurcholis. Gambaran Tingkat Kecemasan Pasien TB Paru di Poli Paru RSUD Kardinah Kota Tegal. Juru Rawat J Update Keperawatan. 2024;4(2):66-73. DOI: 10.31983/juk.v4i2.12474
36. Rajeswari R, Muniyandi M, Balasubramanian R, Narayanan PR. Perceptions of tuberculosis patients about their physical, mental and social well-being: a field report from south India. Soc Sci Med. 2005;60(8):1845-53. DOI: 10.1016/j.socscimed.2004.08.024; PMID: 15686814
37. Anggriani A, Djabir YY, Nurhaeni, Hakim N, Rahyunita, Usman SAA. Penerapan Pelayanan Informasi Obat di Beberapa Puskesmas Kota Makassar. Majalah Farmasi Farmakologi. 2022;26(3):111–3. DOI: 10.1155/2017/8310636
38. Sari SP, Funna ED, Septini R. Cost-utility analysis of tuberculosis patients with directly observed treatment and self-administered treatment in an army hospital, Indonesia. Pharm Sci Asia. 2020;47(3):253–61. DOI: 10.29090/psa.2020.03.019.0019
Authors
Copyright (c) 2025 Baha Udin, Yusransyah Yusransyah, Saepudin Saepudin

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.