Carbapenem Resistant Enterobacteriaceae in Africa
Abstract
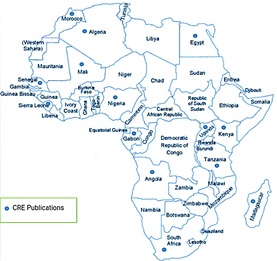
Carbapenems are regarded as unique among the β-lactam antibiotics due to their broad spectrum of activity and ability to resist β-lactamase hydrolysis. Carbapenems are the only β-lactam antibiotics with efficacy in severe infections caused by extended-spectrum beta-lactamase (ESBL) producing bacteria. However, recent reports of carbapenem resistance particularly among members of Enterobacteriaceae that are responsible for diseases such as gastrointestinal infections, septicemia, pneumonia, meningitis, peritonitis as well as urinary tract infections, call for concerns. In Africa, the problem of carbapenem-resistant Enterobacteriaceae (CRE) is aggravated by factors such as the high rate of infections, poor diagnostic tools, sub-optimal disease surveillance, and abuse of antibiotics. Besides, the problem of CRE in Africa is understudied. This review distills available literature on the spread of CRE in Africa, CRE genes in circulation, and the need to pay attention to this emerging threat to lives in developing countries.
Full text article
References
Bathoorn, E., Friedrich, A.W., Zhou, K., Arends, J.P., Borst, D.M., Grundmann, H., & Rossen, J.W. (2013). Latent Introduction to the Netherlands of Multiple Antibiotic Resistance Including NDM-1 After Hospitalisation in Egypt, August 2013. Euro Surveillance, 18(42), 20610. doi:10.2807/1560-7917.es2013.18.42.20610
Brink, A., Coetzee, J., Clay, C., Corcoran, C., van Greune, J., Deetlefs, J.D., Nutt, L., Feldman, C., Richards, G., Nordmann, P., & Poirel, L. (2012). South African Medical Journal, 102(7), 599-601. doi:10.7196/samj.5789
Chika, E., Malachy, U., Ifeanyichukwu, I.E., Peter, E., Thaddeus, G., & Charles, E. (2014). Phenotypic Detection of Metallo-β-Lactamase ( MBL ) Enzyme in Enugu , Southeast Nigeria. American Journal of Biological, Chemical and Pharmaceutical Sciences, 2(2), 1-6.
Codjoe, F.S. & Donkor, E.S. (2017). Carbapenem Resistance: A Review. Medical Sciences, 6(1), 1. doi:10.3390/medsci6010001
Codjoe, F.S., Donkor, E.S., Smith, T.J., & Miller, K. (2019). Phenotypic and Genotypic Characterization of Carbapenem-Resistant Gram-Negative Bacilli Pathogens From Hospitals in Ghana. Microbial Drug Resistance, 25(10), 1449-1457. doi:10.1089/mdr.2018.0278
Dortet, L., Poirel, L., & Nordmann, P. (2014). Worldwide Dissemination of the NDM-type Carbapenemases in Gram-negative Bacteria. BioMed Research International, 2014, 249856. doi:10.1155/2014/249856
Hawkey, P.M. & Livermore, D.M. (2012). Carbapenem Antibiotics for Serious Infections. The BMJ, 344, 3236. doi:10.1136/bmj.e3236
Iovleva, A. & Doi, Y. (2017). Carbapenem-Resistant Enterobacteriaceae. Clinics in Laboratory Medicine, 37(2), 303-315. doi:10.1016/j.cll.2017.01.005
Kariuki, S. & Dougan, G. (2014). Antibacterial resistance in sub‐Saharan Africa: an underestimated emergency. Annals of the New York Academy of Sciences, 1323(1), 43-55. doi:10.1111/nyas.12380
Kelly, A.M., Mathema, B., Larson, E.L. (2017). Carbapenem-resistant Enterobacteriaceae in the Community: A Scoping Review. International Journal of Antimicrobial Agents, 50(2), 127-134. doi:10.1016/j.ijantimicag.2017.03.012
Kieffer, N., Nordmann, P., Aires-de-Sousa, M., & Poirel, L. (2016). High Prevalence of Carbapenemase-Producing Enterobacteriaceae Among Hospitalized Children in Luanda, Angola. Antimicrobial Agents and Chemotherapy, 60(10), 6189-6192. doi:10.1128/aac.01201-16
Knapp, K.M. & English, B.K. (2001). Carbapenems. Seminars in Pediatric Infectious Diseases, 12(3), 175-185. doi:10.1053/spid.2001.24093
Ktari, S., Arlet, G., Mnif, B., Gautier, V., Mahjoubi, F., Jmeaa, M.B., Bouaziz, M., & Hammami, A. (2006). Emergence of Multidrug-Resistant Klebsiella Pneumoniae Isolates Producing VIM-4 Metallo-Beta-Lactamase, CTX-M-15 Extended-Spectrum Beta-Lactamase, and CMY-4 AmpC Beta-Lactamase in a Tunisian University Hospital. Antimicrobial Agents and Chemotherapy, 50(12), 4198-4201. doi:10.1128/aac.00663-06
Kumarasamy, K.K., Toleman, M.A., Walsh, T.R., Bagaria, J., Butt, F., Balakrishnan, R., Chaudhary, U., Coumith, M., Giske, C.G., Irfan, S., Khrisnan, P., Kumar, A.V., Maharjan, S., Mushtaq, S., Noorie, T., Paterson, D.L., Pearson, A., Perry, C., Pike, R., Rao, B., Ray, U., Sarma, J.B., Sharma, M., Sheridan, E., Thirunarayan, M.A., Turton, J., Upadhyay, S., Warner, M., Welfare, W., Livermore, D.M., & Woodford, N. (2010). The Lancet Infectious Diseases, 10(9), 597-602. doi:10.1016/S1473-3099(10)70143-2
Lowman, W., Sriruttan, C., Nana, T., Bosman, N., Duse, A., Venturas, J., Clay, C., & Coetzee, J. (2011). NDM-1 Has Arrived: First Report of a Carbapenem Resistance Mechanism in South Africa. South African Medical Journal, 101(12), 873-875.
Magiorakos, A.P., Burns, K., Rodriguez-Bano, J., Borg, M., Daikos, G., Dumpis, U., Lucet, J.C., Moro, M.L., Tacconelli, E., Skov-Simonsen, G., Szilagyi, E., Voss, A., & Weber, J.T. (2017). Infection prevention and control measures and tools for the prevention of entry of carbapenem-resistant Enterobacteriaceae into healthcare settings: guidance from the European Centre for Disease Prevention and Control. Antimicrobial Resistance and Infection Control, 6, 113. doi:10.1186/s13756-017-0259-z
Manyi-Loh, C., Mamphweli, S., Meyer, E., & Okoh, A. (2018). Antibiotic Use in Agriculture and Its Consequential Resistance in Environmental Sources: Potential Public Health Implications. Molecules, 23(4), 795. doi:10.3390/molecules23040795
Maphumulo, W.T. & Bhengu, B.R. (2019). Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curationis, 42(1), 1901. doi:10.4102/curationis.v42i1.1901
Mitgang, E.A., Hartley, D.M., Malchione, M.D., Koch, M., & Goodman, J.L. (2018). Review and Mapping of Carbapenem-Resistant Enterobacteriaceae in Africa: Using Diverse Data to Inform Surveillance Gaps. International Journal of Antimicrobial Agents, 52(3), 372-384. doi:10.1016/j.ijantimicag.2018.05.019
Moussounda, M., Diene, S.M., Dos Santos, S., Goudeau, A., Francois, P., van der Mee-Marquet, N. (2017). Emergence of Bla NDM-7-Producing Enterobacteriaceae in Gabon, 2016. Emerging Infectious Diseases, 23(2), 356-358. doi:10.3201/eid2302.161182
Muggeo, A., Guillard, T., Klein, F., Reffuveille, F., Francois, C., Babosan, A., Bajolet, O., Bertrand, X., de Champs, C., & CarbaFrEst Group. Journal of Global Antimicrobial Resistance, 13, 98-103. doi:10.1016/j.jgar.2017.10.023
Mushi, M.F., Mshana, S.E., Imirzalioglu, C., & Bwanga, F. (2014). Carbapenemase Genes among Multidrug Resistant Gram Negative Clinical Isolates from a Tertiary Hospital in Mwanza, Tanzania. BioMed Research International, 2014, 303104. doi:10.1155/2014/303104
Ogbolu, D.O. & Webber, M.A. (2014). High-level and Novel Mechanisms of Carbapenem Resistance in Gram-negative Bacteria From Tertiary Hospitals in Nigeria. International Journal of Antimicrobial Agents, 43(5), 412-417. doi:10.1016/j.ijantimicag.2014.01.014
Okeke, I.N. (2016). Laboratory systems as an antibacterial resistance containment tool in Africa. African Journal of Laboratory Medicine, 5(3), 497. doi:10.4102/ajlm.v5i3.497
Okoche, D., Asiimwe, B.B., Katabazi, F.A., Kato, L., & Najjuka, C.F. (2015). Prevalence and Characterization of Carbapenem-Resistant Enterobacteriaceae Isolated From Mulago National Referral Hospital, Uganda. PLoS One, 10(8), 0135745. doi:10.1371/journal.pone.0135745
Oladipo, E.K., Ajibade, O.A., Adeosun, I.J., Awoyelu, E.H., Akinade, S.B., Alabi, O.A., & Ayilara, O.A. (2018). Antimicrobial resistance pattern of clinical isolates of Pseudomonas aeruginosa and Escherichia coli on carbapenems. African Journal of Clinical and Experimental Microbiology, 19(3), 159-164. doi:10.4314/ajcem.v19i3.1
Papp-Wallace, K.M., Endimiani, A., Taracila, M.A., & Bonomo, R.A. (2011). Carbapenems: Past, Present, and Future. Antimicrobial Agents and Chemotherapy, 55(11), 4943-4960. doi:10.1128/AAC.00296-11
Perovic, O., Britz, E., Chetty, V., & Singh-Moodley, A. (2016). Molecular detection of carbapenemase-producing genes in referral Enterobacteriaceae in South Africa: A short report. South African Medical Journal, 106(10), 975-977. doi:10.7196/SAMJ.2016.v106i10.11300
Poirel, L., Revathi, G., Bernabeu, S., & Nordmann, P. (2011). Detection of NDM-1-producing Klebsiella Pneumoniae in Kenya. Antimicrobial Agents and Chemotherapy, 55(2), 934-936. doi:10.1128/aac.01247-10
Rawat, D. & Najr, D. (2010). Extended-spectrum β-lactamases in Gram Negative Bacteria. Journal of Global Infectious Diseases, 2(3), 263-274. doi:10.4103/0974-777X.68531
Robin, F., Aggoune-Khinache, N., Delmas, J., Naim, M., & Bonnet, R. (2010). Novel VIM Metallo-Beta-Lactamase Variant From Clinical Isolates of Enterobacteriaceae From Algeria. Antimicrobial Agents and Chemotherapy, 54(1), 466-470. doi:10.1128/aac.00017-09
Rodriguez-Martinez, J.M., Nordmann, P., Fortineau, N., & Poirel, L. (2010). VIM-19, a Metallo-Beta-Lactamase With Increased Carbapenemase Activity From Escherichia Coli and Klebsiella Pneumoniae. Antimicrobial Agents and Chemotherapy, 54(1), 471-476. doi:10.1128/aac.00458-09
Sangare, S.A., Rondinaud, E., Maataoui, N., Maiga, A.I., Guindo, I., Maiga, A., Camara, N., Dicko, O.A., Dao, S., Diallo, S., Bougoudogo, F., Andremont, A., Maiga, I.I., Armand-Lefevre, L. (2017). Very High Prevalence of Extended-Spectrum Beta-Lactamase-Producing Enterobacteriaceae in Bacteriemic Patients Hospitalized in Teaching Hospitals in Bamako, Mali. PLoS One, 12(2), 0172652. doi:10.1371/journal.pone.0172652
Sekyere, J.O., Govinden, U., & Essack, S. (2016). The Molecular Epidemiology and Genetic Environment of Carbapenemases Detected in Africa. Microbial Drug Resistance, 22(1), 59-68. doi:10.1089/mdr.2015.0053
Tadesse, B.T., Ashley, E.A., Ongarello, S., Havumaki, J., Wijegoonewardena, M., Gonzales, I.J., & Dittrich, S. (2017). Antimicrobial Resistance in Africa: A Systematic Review. BMC Infectious Diseases, 17(1), 616. doi:10.1186/s12879-017-2713-1
Tischendorf, J., de Avila, R.A., & Safdar, N. (2016). Risk of Infection Following Colonization With Carbapenem-Resistant Enterobactericeae: A Systematic Review. American Journal of Infection Control, 44(5), 539-543. doi:10.1016/j.ajic.2015.12.005
Ventola, C.L. (2015). The Antibiotic Resistance Crisis: Part 1: Causes and Threats. Pharmacy and Therapeutics, 40(4), 277-283.
Yusuf, I., Yusha’u, M., Sharif, A.A., Getso, M.I., Yahaya, H., Bala, J.A., Aliyu, I.A., & Haruna, M. (2012). Detection of metallo betalactamases among gram negative bacterial isolates from Murtala Muhammad Specialist Hospital, Kano and Almadina Hospital Kaduna, Nigeria. Bayero Journal of Pure and Applied Sciences, 5(2), 84-88. doi:10.4314/bajopas.v5i2.15
Zhanel, G.G., Wiebe, R., Dilay, L., Thomson, K., Rubinstein, E., Hoban, D.J., Noreddin, A.M., & Karlowsky, J.A. (2007). Comparative Review of the Carbapenems. Drugs, 67(7), 1027-1052. doi:10.2165/00003495-200767070-00006
Authors
Copyright (c) 2020 Bashar Haruna Gulumbe, Olumide Ajibola

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.