Advantages of Herbal Over Allopathic Medicine in the Management of Kidney and Urinary Stones Disease
Abstract
Kidney and urinary stone disease (Nephrolithiasis and urolithiasis) are the condition where urinary stones or calculi are formed in the urinary tract. The problem of urinary stones is very ancient; these stones are found in all parts of the urinary tract, kidney, ureters, and the urinary bladder and may vary considerably in size. It is a common disease estimated to occur in approximately 12% of the population, with a recurrence rate of 70-81% in males and 47-60% in females. The treatment of kidney and urinary stone diseases such as a western (allopathy) medicine and surgery is now in trends. However, most people preferred plant-based (herbal) therapy because of the overuse of allopathic drugs, which results in a higher incidence rate of adverse or severe side effects. Therefore, people every year turn to herbal therapy because they believe plant-based medicine is free from undesirable side effects, although herbal medicines are generally considered to be safe and effective. In the present article, an attempt has been made to emphasize an herbal therapy is better than allopathic therapy for the management of the kidney and urinary stone disease.
Full text article
References
Afsar, B., Kiremit, M.C., Sag, A.A., Tarim, K., Acar, O., Esen, T., Solak, Y., Covic, A., & Kanbay, M. (2016). The role of sodium intake in nephrolithiasis: epidemiology, pathogenesis, and future directions. European Journal of Internal Medicine, 35, 16-19. doi:10.1016/j.ejim.2016.07.001
Ahmed, A.F., Gabr, A.H., Emara, A.A., Ali, M., Abdel-Aziz, A.S., & Alshahrani, S. (2015). Factors predicting the spontaneous passage of a ureteric calculus of ⩽10 mm. Arab Journal of Urology, 13(2), 84-90. doi:10.1016/j.aju.2014.11.004
Albert, A., Tiwari, V., Paul, E., Ganesan, D., Ayyavu, M., Kujur, R., Ponnusamy, S., Shanmugam, K., Saso, L., & Sadasivam, S.G. (2017). Expression of heterologous oxalate decarboxylase in HEK293 cells confers protection against oxalate induced oxidative stress as a therapeutic approach for calcium oxalate stone disease. Journal of Enzyme Inhibition and Medicinal Chemistry, 32(1), 426-433. doi:10.1080/14756366.2016.1256884
Arya, P., Pandey, S., & Verma, V. (2017). Kidney stone formation and use of medicinal plants as anti-urolithiatic agents. Universal Journal of Pharmaceutical Research, 2(4), 43-48. doi:10.22270/ujpr.v2i4.RW1
Aune, D., Mahamat-Saleh, Y., Norat, T., & Riboli, E. (2018). Body fatness, diabetes, physical activity and risk of kidney stones: a systematic review and meta-analysis of cohort studies. European Journal of Epidemiology, 33(11), 1033-1047. doi:10.1007/s10654-018-0426-4
Aziz, F.M. &Hassan, D.H. (2020). Radish Juice Promote Kidney Stone Deposition in Ethylene Glycol-induced Urolithiasis in Rats. Cihan University-Erbil Scientific Journal, 4(1), 57-61. doi:10.24086/cuesj.v4n1y2020
Bultitude, M., Smith, D., & Thomas, K. (2016). Contemporary Management of Stone Disease: The New EAU Urolithiasis Guidelines for 2015. European Urology, 69(3), 483-483. doi:10.1016/j.eururo.2015.08.010
Çakıroğlu, B., Eyyupoğlu, E., Hazar, A.I., Uyanik, B.S., & Nuhoğlu, B. (2016). Metabolic assessment of recurrent and first renal calcium oxalate stone formers. Archivio Italiano di Urologia e Andrologia, 88(2), 101-105. doi:10.4081/aiua.2016.2.101
Chaveau, P., Aparicio, M., Belizzi, V., Campbell, K., Hong, X., Johansson, L., Kolko, A., Molina, P., Sezer, S., Wanner, C., Ter Wee, P.M., Teta, D., Fouque, D., Carrero, J.J., & European Renal Nutrition (ERN) Working Group of the European Renal Association–European Dialysis Transplant Association (ERA-EDTA). (2018). Mediterranean diet as the diet of choice for patients with chronic kidney disease. Nephrology Dialysis Transplantation, 33(5), 723-735. doi:10.1093/ndt/gfx085
Chen, K., Chen, D., Lan, C., Liang, X., Zeng, T., Huang, J., Duan, X., Kong, Z., Li, S., Tiselius, H.G., Gurioli, A., Lu, X., Zeng, G., & Wu, W. (2018). Does green tea consumption increase urinary oxalate excretion? Results of a prospective trial in healthy men. International Urology and Nephrology, 50, 29-33. doi:10.1007/s11255-017-1720-x
Cloutier, J., Villa, L., Traxer, O., & Daudon, M. (2015). Kidney stone analysis: "Give me your stone, I will tell you who you are!". World Journal of Urology, 33(2), 157-169. doi:10.1007/s00345-014-1444-9
Coe, F.L., Worcester, E.M. & Evan, A.P. (2016). Idiopathic hypercalciuria and formation of calcium renal stones. Nature Reviews Nephrology, 12(9), 519-533. doi:10.1038/nrneph.2016.101
Courbebaisse, M., Prot-Bertoye, C., Bertocchio, J.P., Baron, S., Maruani, G., Briand, S., Daudon, M., & Houillier, P. (2017). [Nephrolithiasis of adult: From mechanisms to preventive medical treatment]. Revue Medicale Internationale, 38(1), 44-52. doi:10.1016/j.revmed.2016.05.013
Das, M. & Malipeddi, H. (2016). Antiurolithiatic activity of ethanol leaf extract of Ipomoea eriocarpa against ethylene glycol-induced urolithiasis in male Wistar rats. Indian Journal of Pharmacology, 48(3), 270-274. doi:10.4103/0253-7613.182886
Daudon, M., Frochot, V., Bazin, D., & Jungers, P. (2018). Drug-Induced Kidney Stones and Crystalline Nephropathy: Pathophysiology, Prevention and Treatment. Drugs, 78(2), 163-201. doi:10.1007/s40265-017-0853-7
Duan, X., Zhang, T., Ou, L., Kong, Z., Wu, W., & Zeng, G. (2020). 1 H NMR-based metabolomic study of metabolic profiling for the urine of kidney stone patients. Urolithiasis, 48(1), 27-35. doi:10.1007/s00240-019-01132-2
Evan, A.P., Worcester, E.M., Coe, F.L., Williams, J., & Lingeman, J.E. (2015). Mechanisms of human kidney stone formation. Urolithiasis, 43 Suppl 1(0 1), 19-32. doi:10.1007/s00240-014-0701-0
Ferraro, P.M., Marano, R., Primiano, A., Gervasoni, J., Bargagli, M., Rovere, G., Bassi, & Gambaro, G. (2019). Stone composition and vascular calcifications in patients with nephrolithiasis. Journal of Nephrology, 32(4), 589-594. doi:10.1007/s40620-019-00619-w
Ferraro, P.M., Curhan, G.C., D’Addessi, A., & Gambaro, G. (2017). Risk of recurrence of idiopathic calcium kidney stones: analysis of data from the literature. Journal of Nephrology, 30(2), 227-233. doi:10.1007/s40620-016-0283-8
Fisang, C., Anding, R., Müller, S.C., Latz, S., & Laube, N. (2015). Urolithiasis--an interdisciplinary diagnostic, therapeutic and secondary preventive challenge. Deutsches Ärzteblatt International, 112(6), 83-91. doi:10.3238/arztebl.2015.0083
Gambaro, G., Croppi, E., Bushinsky, D., Jaeger, P., Cupisti, A., Ticinesi, A., Mazzaferro, S., D’Addessi, A., & Ferraro, P.M. (2017). The Risk of Chronic Kidney Disease Associated with Urolithiasis and its Urological Treatments: A Review. Journal of Urology, 198(2), 268-273. doi:10.1016/j.juro.2016.12.135
Gambaro, G., Croppi, E., Coe, F., Lingeman, J., Moe, O., Worcester, E., Buchholz, N., Bushinsky, D., Curhan, G.C., Ferraro, P.M., Fuster, D., Goldfarb, D.S., Heilberg, I.P., Hess, B., Lieske, J., Marangella, M., Milliner, D., Preminger, G.M., Santos J.M.R., Sakhaee, K., Sarica, K., Siener, R., Strazzullo, P., Williams, J.C., & Consensus Conference Group. (2016). Metabolic diagnosis and medical prevention of calcium nephrolithiasis and its systemic manifestations: a consensus statement. Journal of Urology, 29(6), 715-734. doi:10.1007/s40620-016-0329-y
Giardina, S., Scilironi, C., Michelotti, A., Samuele, A., Borella, F., Daglia, M., & Marzatico, F. (2014). In vitro anti-inflammatory activity of selected oxalate-degrading probiotic bacteria: potential applications in the prevention and treatment of hyperoxaluria. Journal of Food Science, 79(3), M384-390. doi:10.1111/1750-3841.12344
Green, W. & Ratan, H. (2013). Molecular mechanisms of urolithiasis. Urology, 81(4), 701-704. doi:10.1016/j.urology.2012.12.039
Han, H., Segal, A.M., Seifter, J.L., & Dwyer, J.T. (2015). Nutritional Management of Kidney Stones (Nephrolithiasis). Clinical Nutrition Research, 4(3), 137-152. doi:10.7762/cnr.2015.4.3.137
Hollingsworth, J.M., Canales, B.K., Rogers, M.A.M., Sukumar, S., Yan, P., Kuntz, G.M., & Dahm, P. (2016). Alpha blockers for treatment of ureteric stones: systematic review and meta-analysis. BMJ, 355, i6112. doi:10.1136/bmj.i6112
Holmes, R.P., Knight, J., & Assimos, D.G. (2016). Lowering urinary oxalate excretion to decrease calcium oxalate stone disease. Urolithiasis, 44(1), 27-32. doi:10.1007/s00240-015-0839-4
Jung, H. & Osther, P.J.S. (2015). Acute management of stones: When to treat or not to treat? World Journal of Urology, 33, 203-211. doi:10.1007/s00345-014-1353-y
Kanlaya, R., Singhto, N., & Thongboonkerd, V. (2016). EGCG decreases binding of calcium oxalate monohydrate crystals onto renal tubular cells via decreased surface expression of alpha-enolase. Journal of Biological Inorganic Chemistry, 21(3), 339-346. doi:10.1007/s00775-016-1344-0
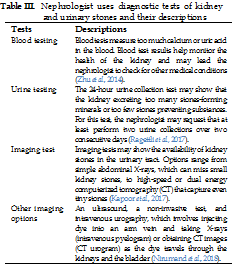
Kapoor, D., Vyas, R.B., & Dadarwal, D. (2017). Nephrolithiasis – an updated review in relation to diagnosis, prevention and treatment. Journal of Translational Medicine and Research, 1(2), 37-42. doi:10.15406/oajtmr.2017.01.00009
Khan, S.R., Pearle, M.S., Robertson, W.G., Gambaro, G., Canales, B.K., Doizi, S., Traxer, O., & Tiselius, H.G. (2016). Kidney stones. Nature Reviews Disease Primers, 2, 16008. doi:10.1038/nrdp.2016.8
Kummer, A.E., Grams, M., Lutsey, P., Chen, Y., Matsushita, K., Kottgen, A., Folsom, A.R., & Coresh, J. (2015). Nephrolithiasis as a Risk Factor for CKD: The Atherosclerosis Risk in Communities Study. Clinical Journal of the American Society of Nephrology, 10(11), 2023-2029. doi:10.2215/CJN.10111014
McTavish, R.K., Richard, L., McArthur, E., Shariff, S.Z., Acedillo, R., Parikh, C.R., Wald, R., Wilk, P., & Garg, A.X. (2018). Association Between High Environmental Heat and Risk of Acute Kidney Injury Among Older Adults in a Northern Climate: A Matched Case-Control Study. American Journal of Kidney Diseases, 71(2), 200-208. doi:10.1053/j.ajkd.2017.07.011
Nirumand, M.C., Hajialyani, M., Rahimi, R., Farzaei, Zingue, S., Nabavi, S.M., & Bishayee, A. (2018). Dietary Plants for the Prevention and Management of Kidney Stones: Preclinical and Clinical Evidence and Molecular Mechanisms. International Journal of Molecular Sciences, 19(3), 765. doi:10.3390/ijms19030765
Pathan, S.A., Mitra, B., & Cameron, P.A. (2018). A Systematic Review and Meta-analysis Comparing the Efficacy of Nonsteroidal Anti-inflammatory Drugs, Opioids, and Paracetamol in the Treatment of Acute Renal Colic. European Urology, 73(4), 583-595. doi:10.1016/j.eururo.2017.11.001
Pearle, M.S., Goldfarb, D.S., Assimos, D.G., Curhan, G., Denu-Ciocca, C.J., Matlaga, B.R., Monga, M., Penniston, K.L., Preminger, G.M., Turk, T.M.T., White, J.R., & American Urological Association. (2014). Medical management of kidney stones: AUA guideline. Journal of Urology, 192(2), 316-324. doi:10.1016/j.juro.2014.05.006
Pickard, R., Starr, K., MacLennan, G., Lam, T., Thomas, R., Burr, J., McPherson, G., McDonald, A., Anson, K., N’Dow, J., Burgess, N., Clark, T., Kilonzo, M., Gillies, K., Shearer, K., Boachie, C., Cameron, S., Norrie, J., & McClinton, S. (2015). Medical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trial. The Lancet, 386(9991), 341-349. doi:10.1016/S0140-6736(15)60933-3
Podzik, A., Maalouf, N., Letavernier, E., Brocheriou, I., Body, J.J., Vervaet, B., Haute, C.V., Noels, J., Gadisseur, R., Castiglione, V., Cotton, F., Gambaro, G., Daudon, M., & Sakhaee, K. (2019). Meeting report of the "Symposium on kidney stones and mineral metabolism: calcium kidney stones in 2017". Journal of Nephrology, 32(5), 681-698. doi:10.1007/s40620-019-00587-1
Prabhu, V.V., Sathyamurthy, D., Ramasamy, A., Das, S., Anuradha, M., & Pachiappan, S. (2016). Evaluation of protective effects of diosmin (a citrus flavonoid) in chemical-induced urolithiasis in experimental rats. Pharmaceutical Biology, 54(9), 1513-1521. doi:10.3109/13880209.2015.1107105
Prezioso, D., Strazzullo, P., Lotti, T., Bianchi, G., Borghi, L., Caione, P., Carini, M., Caudarella, R., Ferraro, M., Gambaro, G., Gelosa, M., Guttilla, A., Illiano, E., Martino, M., Meschi, T., Messa, P., Miano, R., Napodano, G., Nouvenne, A., Rendina, D., Rocco, F., Rosa, M., Sanseverino, R., Salerno, A., Spatafora, S., Tasca, A., Ticinesi, A., Travaglini, F., Trinchieri, A., Vespasiani, G., & Zattoni, F. (2016). ERRATUM: Dietary treatment of urinary risk factors for renal stone formation. A review of CLU Working Group. Archivio Italiano di Urologia e Andrologia, 88(1), 76. doi:10.4081/aiua.2016.1.76
Primarizky, H., Yuniari, W.M., & Lukiswanto, B.S. (2016). Benefits of pomegranate (Punica granatum Linn) fruit extracts to weight changes, total protein, and uric acid in white rats (Rattus norvegicus) as an animal model of acute renal failure. Veterinary World, 9(11), 1269-1274. doi:10.14202/vetworld.2016.1269-1274
Ragettli, M.S., Vicedo-Cabrera, A.M., Schindler, C., & Röösli, M. (2017). Exploring the association between heat and mortality in Switzerland between 1995 and 2013. Environmental Research, 158, 703-709. doi:10.1016/j.envres.2017.07.021
Rodger, F., Roditi, G., & Aboumarzouk, O.M. (2018). Diagnostic Accuracy of Low and Ultra-Low Dose CT for Identification of Urinary Tract Stones: A Systematic Review. Urologia Internationalis, 100(4), 375-385. doi:10.1159/000488062
Rodgers, A., Mokoena, M., Durbach, I., Lazarus, J., de Jager, S., Ackermann, H., Breytenbach, I., Okada, A., Usami, M., Hirose, Y., Ando, R., Yasui, T., & Kohri, K. (2016). Do teas rich in antioxidants reduce the physicochemical and peroxidative risk factors for calcium oxalate nephrolithiasis in humans? Pilot studies with Rooibos herbal tea and Japanese green tea. Urolithiasis, 44(4), 299-310. doi:10.1007/s00240-015-0855-4
Ross, M.E., Vicedo-Cabrera, A.M., Kopp, R.E., Song, L., Goldfarb, D.S., Pulido, J., Warner, S., Furth, S.L., & Tasian, G.E. (2018). Assessment of the combination of temperature and relative humidity on kidney stone presentations. Environmental Research, 162, 97-105. doi:10.1016/j.envres.2017.12.020
Roudakova, K. & Monga, M. (2014). The evolving epidemiology of stone disease. Indian Journal of Urology, 30(1), 44-48. doi:10.4103/0970-1591.124206
Scales, C.D., Tasian, G.E., Schwaderer, A.L., Goldfarb, D.S., Star, R.A., & Kirkali, Z. (2016). Urinary Stone Disease: Advancing Knowledge, Patient Care, and Population Health. Clinical Journal of the American Society of Nephrology, 11(7), 1305-1312. doi:10.2215/cjn.13251215
Shang, W., Li, Y., Ren, Y., Yang, Y., Li, H., & Dong, J. (2017). Nephrolithiasis and risk of hypertension: a meta-analysis of observational studies. BMC Nephrology, 18, 344. doi:10.1186/s12882-017-0762-8
Sharifiyan, F., Movahedian-Attar, A., Nili, N., & Asgary, S. (2016). Study of pomegranate (Punica granatum L.) peel extract containing anthocyanins on fatty streak formation in the renal arteries in hypercholesterolemic rabbits. Advanced Biomedical Research, 5, 8. doi:10.4103/2277-9175.175241
Shavit, L., Ferraro, P.M., Johri, N., Robertson, W., Walsh, S.B., Moochhala, S., & Unwin, R. (2015). Effect of being overweight on urinary metabolic risk factors for kidney stone formation. Nephrology Dialysis Transplantation, 30(4), 607-613. doi:10.1093/ndt/gfu350
Skolarikos, A., Straub, M., Knoll, T., Sarica, K., Seitz, C., Petřík, A., & Türk, C. (2015). Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines. European Urology, 67(4), 750-763. doi:10.1016/j.eururo.2014.10.029
Smith-Bindman, R., Aubin, C., Bailitz, J., Bengiamin, R.N., Camargo, C.A., Corbo, J., Dean, A.J., Goldstein, R.B., Griffey, R.T., Jay, G.D., Kang, T.L., Kriesel, D.R., Ma, O.J., Mallin, M., Manson, W. Melnikow, J., Miglioretti, D.L., Miller, S.K., Mills, L.D., Miner, J.R., Moghadassi, M. Noble, V.E., Press, G.M., Stoller, M.L., Valencia, V.E., Wang, J., Wang, R.C., & Cummings, S.R. (2014). Ultrasonography versus Computed Tomography for Suspected Nephrolithiasis. The New England Journal of Medicine, 371(12), 1100-1110. doi:10.1056/NEJMoa1404446
Spatola, L., Ferraro, P.M., Gambaro, G., Badalamenti, S., & Dauriz, M. (2018). Metabolic syndrome and uric acid nephrolithiasis: insulin resistance in focus. Metabolism: Clinical and Experimental, 83, 225-233. doi:10.1016/j.metabol.2018.02.008
Strepper, N.M. (2018). Asymptomatic Renal Stones-to Treat or Not to Treat. Current Urology Reports, 19(5), 29. doi:10.1007/s11934-018-0782-3
Tavasoli, S., Alebouyeh, M., Naji, M., Majd, G.S., Nashtaei, M.S., Broudmandnia, N., & Basiri, A. (2020). Association of intestinal oxalate-degrading bacteria with recurrent calcium kidney stone formation and hyperoxaluria: a case-control study. BJU International, 125(1), 133-143. doi:10.1111/bju.14840
Ticinesi, A., Nouvenne, A., & Meschi, T. (2019). Gut microbiome and kidney stone disease: not just an Oxalobacter story. Kidney International, 96(1), 25-27. doi:10.1016/j.kint.2019.03.020
Ticinesi, A., Guerra, A., Allegri, F., Nouvenne, A., Cervellin, G., Maggio, M., Lauretani, F., Borghi, L., & Meschi, T. (2018). Determinants of calcium and oxalate excretion in subjects with calcium nephrolithiasis: the role of metabolic syndrome traits. Journal of Nephrology, 31, 395-403. doi:10.1007/s40620-017-0453-3
Türk, C., Petřík, A., Sarica, K., Seitz, C., Skolarikos, A., Straub, M., & Knoll, T. (2016). EAU Guidelines on Diagnosis and Conservative Management of Urolithiasis. European Urology, 69(3), 468-474. doi:10.1016/j.eururo.2015.07.040
Unno, R., Kawabata, T., Taguchi, K., Sugino, T., Hamamoto, S., Ando, R., Okada, A., Kohri, K., Yoshimori, T., & Yasui, T. (2020). Deregulated MTOR (mechanistic target of rapamycin kinase) is responsible for autophagy defects exacerbating kidney stone development. Autophagy, 16(4), 709-723. doi:10.1080/15548627.2019.1635382
Vicedo-Cabrera, A.M., Goldfarb, D.S., Kopp, R.E., Song, L., & Tasian, G.E. (2020). Sex differences in the temperature dependence of kidney stone presentations: a population-based aggregated case-crossover study. Urolithiasis, 48(1), 37-46. doi:10.1007/s00240-019-01129-x
Wang, H., Man, L.B., Huang, G.L., Li, G.Z., & Wang, J.W. (2016). Comparative efficacy of tamsulosin versus nifedipine for distal ureteral calculi: a meta-analysis. Drug Design, Development, and Therapy, 10, 1257-1265. doi:10.2147/DDDT.S99330
Wijarnpreecha, K., Lou, S., Panjawatanan, P., Sanguankeo, A., Pungpapong, S., Lukens, F.J., & Ungprasert, P. (2018). Nonalcoholic Fatty Liver Disease and Urolithiasis. A Systematic Review and Meta-Analysis. Journal of Gastrointestinal and Liver Diseases, 27(4), 427-432. doi:10.15403/jgld.2014.1121.274.nac
Yiu, A.J., Callaghan, D., Sultana, R., & Bandyopadhyay, B.C. (2015). Vascular Calcification and Stone Disease: A New Look towards the Mechanism. Journal of Cardiovascular Development and Disease, 2(3), 141-164. doi:10.3390/jcdd2030141
Zhu, W., Xu, Y.F., Feng, Y., Peng, B., Che, J.P., Liu, M., & Zheng, J.H. (2014). Prophylactic effects of quercetin and hyperoside in a calcium oxalate stone forming rat model. Urolithiasis, 42(6), 519-526. doi:10.1007/s00240-014-0695-7
Authors
Copyright (c) 2020 Saurabh Nimesh, Vrish Dhwaj Ashwlayan, Rubi Rani, Om Prakash

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.