Association between Drug-Related Problems and Blood Pressure of Hypertensive Patients Admitted to Universitas Sumatera Utara Hospital
Abstract
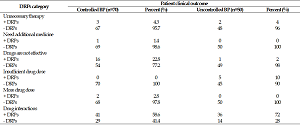
Patients with hypertension usually experience chronic comorbidities and complications that require complex treatment (polypharmacy), which can further cause drug-related problems (DRPs) and interfere with the required clinical outcomes. This study, by using a case-control prospective cross-sectional, aimed to analyze the association between DRPs and blood pressures (BPs) of hypertensive patients admitted to Universitas Sumatera Utara (USU) hospital from July to September 2021. The incidence of DRPs was analyzed and classified according to the Cipolle classification system and reliable literature. Blood pressures of the patients were classified into controlled and uncontrolled BPs. The association between DRPs and BP was analyzed using the Chi-Square test. Most of the patients (57.5%) were female. Their mean age was 59±9.94 (years). The mean incidence of DRPs experienced by the patients was 1.78±0.79. The most frequently occurred DRPs were drug interactions. There was a significant association between the number of DRPs experienced by the patients and their BPs (p=0.02). DRPs are the contributing factor to the uncontrolled BPs of hypertensive patients.
Full text article
References
2. Ridwanah AA, Megatsari H, Laksono AD. Hypertension in Indonesia in 2018: An Ecological Analysis. Indian J Med Forensic Med Toxicol. 2021;15(2):2073-9. doi:10.37506/ijfmt.v15i2.14669
3. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–324. doi:10.1161/hyp.0000000000000066
4. Farha RA, Saleh A, Aburuz S. The impact of drug related problems on health-related quality of life among hypertensive patients in Jordan. Pharm Pract. 2017;15(3):995. doi:10.18549/pharmpract.2017.03.995
5. van Mil JWF, Horvat N, Westerlund T, Zuidlaren IR. Classification for Drug related problems Ann Pharmacother. 2004;38(5):859-67. doi:10.1345/aph.1d182
6. Kusumawardani LA, Andrajati R, Nusaibah A. Drug-related Problems in Hypertensive Patients: A Cross-sectional Study from Indonesia. J Res Pharm Pract. 2020;9(3):140-5. doi:10.4103/jrpp.jrpp_20_16
7. Zhou D, Xi B, Zhao M, Wang L, Veeranki SP. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III Linked Mortality Study. Sci Rep. 2018;8(1):9418. doi:10.1038/s41598-018-27377-2
8. Patil M, Hedaoo RP, Shah RP, Tauseef SM, Marzo RR, Ching SM, et al. Assessment of Health-Related Quality of Life Among Male Patients With Controlled and Uncontrolled Hypertension in Semi Urban India. Inquiry. 2023;60:469580231167010. doi:10.1177/00469580231167010
9. Nasution A, Khairunnisa K, Tanjung HR. Drug Therapy Problems in Management of Hypertensive Outpatients Admitted to Four Indonesia Primary Health Centers. Asian J Pharm Clin Res. 2016;9(1):87-90.
10. Huri HZ, Wee HF. Drug related problems in type 2 diabetes patients with hypertension: a cross-sectional retrospective study. BMC Endocr Disord. 2013;13:2. doi:10.1186/1472-6823-13-2
11. Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: The Clinician's Guide, Second Edition. New York: McGraw-Hill; 2004.
12. Quest DW. Stockley’s drug interactions. 8th edition; Stockley’s drug interactions 2008 pocket companion. Can Fam Physician. 2008;54(7):1025.
13. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-20. doi:10.1001/jama.2013.284427
14. Mahajan R. Joint National Committee 8 report: How it differ from JNC 7. Int J Appl Basic Med Res. 2014;4(2):61-2. doi:10.4103/2229-516x.136773
15. Prihapsari AN, Rahmawati F, Andayani TM. Hubungan antara Drug Related Problems (DRPs) dan Capaian Target Terapi Hipertensi di Puskesmas Kota Yogyakarta [Thesis]. Yogyakarta: Universitas Gadjah Mada; 2016.
16. Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. Resistant Hypertension: Detection, Evaluation, and Management: A Scientific Statement From the American Heart Association. Hypertension.2018;72(5):e53-90. doi:10.1161/hyp.0000000000000084
17. Cobos B, Haskard-Zolnierek K, Howard K. White coat hypertension: improving the patient-health care practitioner relationship. Psychol Res Behav Manag. 2015;8:133–41. doi:10.2147/prbm.s61192
18. Handler J. Managing white-coat effect. J Clin Hypertens. 2008;10(8):649-54. doi:10.1111/j.1751-7176.2008.08064.x
19. Verma N, Rastogi S, Chia YC, Siddique S, Turana Y, Cheng HM, et al. Non-pharmacological management of hypertension. J Clin Hypertens. 2021;23(7):1275-83. doi:10.1111/jch.14236
20. Littlejohn 3rd TW, Majul CR, Olvera R, Seeber M, Kobe M, Guthrie R, et al. Results of treatment with telmisartan-amlodipine in hypertensive patients. J Clin Hypertens. 2009;11(4):207-13. doi:10.1111/j.1751-7176.2009.00098.x
21. Hussein M, Lenjisa JL, Woldu MA, Tegegne GT, Umeta GT, Dins H, et al. Assessment of Drug Related Problems Among Hypertensive Patients on Follow up in Adama Hospital Medical College, East Ethiopia. Clin Pharmacol Biopharm. 2014;3:122. doi:10.4172.2167-065X.1000122
22. Tharanon V, Putthipokin K, Sakthong P. Drug-related problems identified during pharmaceutical care interventions in an intensive care unit at a tertiary university hospital. SAGE Open Med. 2022;10:20503121221090881. doi:10.1177/20503121221090881
23. Bhatty E, Meraj A, Malik M, Imtiaz M, Nasir A, Saleem N, et al. Drug Related Problems Associated with Polypharmacy: A Literature Review. Pak J Pharm. 2017;30(1):10–6.
24. Farha RA, Basheti I, Al Ruz HA, Alsaleh A, AbuRuz S. Assessment of drug-related problems and their impact on blood pressure control in patients with hypertension. Eur J Hosp Pharm. 2016;23(3):126-30. doi:10.1136/ejhpharm-2015-000712
25. Abegaz TM, Tefera YG, Abebe TB. Antihypertensive drug prescription patterns and their impact on outcome of blood pressure in Ethiopia: a hospital-based cross-sectional study. Integr Pharm Res Pract. 2017;6:29–35. doi:10.2147/iprp.s124047
Authors
Copyright (c) 2023 Mutiara Siahaan, Azizah Nasution, Wiryanto Wiryanto, Iksen Iksen

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.