A Review of Antifungal Resistance in West Africa
Abstract
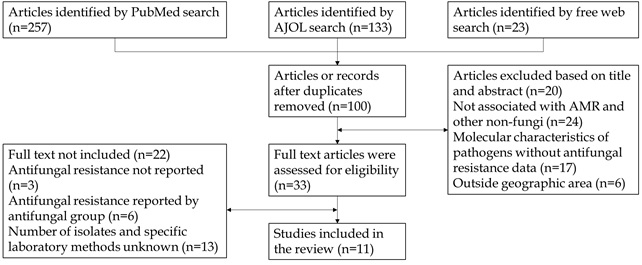
Knowledge of local and regional antimicrobial resistance (AMR) is important for clinical decision-making. However, surveillance capacity for fungal infections let alone antifungal resistance is lacking throughout West Africa, and current antifungal resistance data are sparse. We sought to address this gap by summarizing all available high-quality data on antifungal resistance in West Africa. We searched the PubMed database, African Journals Online archives, and free web searches in October and December 2023 using the terms "antifungal resistance" and "West Africa" to find articles published from 2010 onwards. Only 11 articles were included in our analysis most of which were cross-sectional and descriptive in design; relatively high levels of antifungal resistance (AFR) to commonly used antifungals were reported including (24-75%) resistance to fluconazole and ketoconazole, two of the most frequently-prescribed antifungals in this region. There is a high level of resistance to griseofulvin, ketoconazole, cotrimoxazole, and fluconazole among dermatophyte infections (80-100%) with 100% resistance to amphotericin B, ketoconazole, and fluconazole reported by the invasive fungal disease-causing pathogen Cryptococcus neoformans. Resistance to commonly used anti-fungal drugs is prevalent; raising concern that these drugs may no longer be useful for treating moderate or severe fungal infections in West Africa hence calling for countries to promote acceptance of antimicrobial stewardship as a programmatic strategy not just focused on bacterial resistance but also fungal resistance including pharmacy management, laboratory complete mycological investigations and dissemination of standard fungal susceptibility profiles.
Full text article
References
2. Papon N, Bougnoux ME, d'Enfert C. Tracing the Origin of Invasive Fungal Infections. Trends Microbiol. 2020;28(4):240-2. Doi: 10.1016/j.tim.2020.01.007; PMID: 32044130
3. Firacative C. Invasive fungal disease in humans: are we aware of the real impact? Mem Inst Oswaldo Cruz. 2020;115:e200430. DOI: 10.1590/0074-02760200430; PMCID: PMC7546207; PMID: 33053052
4. Lamoth F, Lockhart SR, Berkow EL, Calandra T. Changes in the epidemiological landscape of invasive candidiasis. J Antimicrob Chemother. 2018;73(suppl_1):i4-13. DOI: 10.1093/jac/dkx444; PMID: 29304207
5. Vitiello A, Ferrara F, Boccellino M, Ponzo A, Cimmino C, Comberiati E, et al. Antifungal Drug Resistance: An Emergent Health Threat. Biomedicines. 2023;11(4):1063. DOI: 10.3390/biomedicines11041063; PMCID: PMC10135621; PMID: 37189681
6. Fisher MC, Alastruey-Izquierdo A, Berman J, Bicanic T, Bignell EM, Bowyer P, et al. Tackling the emerging threat of antifungal resistance to human health. Nat Rev Microbiol. 2022;20(9):557-71. DOI: 10.1038/s41579-022-00720-1; PMCID: PMC8962932; PMID: 35352028
7. Ioannidis K, Papachristos A, Skarlatinis I, Kiospe F, Sotiriou S, Papadogeorgaki E, et al. Do we need to adopt antifungal stewardship programmes?. Eur J Hosp Pharm. 2020;27(1):14-8. DOI: 10.1136/ejhpharm-2017-001467; PMCID: PMC6992971; PMID: 32064083
8. Osherov N, Kontoyiannis DP. The anti-Aspergillus drug pipeline: Is the glass half full or empty? Med Mycol. 2017;55(1):118-24. DOI: 10.1093/mmy/myw060; PMID: 27562862
9. Hoenigl M, Sprute R, Egger M, Arastehfar A, Cornely OA, Krause R, et al. The Antifungal Pipeline: Fosmanogepix, Ibrexafungerp, Olorofim, Opelconazole, and Rezafungin. Drugs. 2021;81(15):1703-29. DOI: 10.1007/s40265-021-01611-0; PMCID: PMC8501344; PMID: 34626339
10. Perfect JR. The antifungal pipeline: a reality check. Nat Rev Drug Discov. 2017;16(9):603-16. DOI: 10.1038/nrd.2017.46; PMCID: PMC5760994; PMID: 28496146
11. Denning DW, Bromley MJ. Infectious Disease. How to bolster the antifungal pipeline. Science. 2015;347(6229):1414-6. DOI: 10.1126/science.aaa6097; PMID: 25814567
12. Rayens E, Norris KA. Prevalence and Healthcare Burden of Fungal Infections in the United States, 2018. Open Forum Infect Dis. 2022;9(1):ofab593. DOI: 10.1093/ofid/ofab593; PMCID: PMC8754384; PMID: 35036461
13. Köhler JR, Hube B, Puccia R, Casadevall A, Perfect JR. Fungi that Infect Humans. Microbiol Spectr. 2017;5(3):10. DOI: 10.1128/microbiolspec.FUNK-0014-2016. PMID: 28597822
14. Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv13. DOI: 10.1126/scitranslmed.3004404; PMID: 23253612
15. Bailly S, Maubon D, Fournier P, Pelloux H, Schwebel C, Chapuis C, et al. Impact of antifungal prescription on relative distribution and susceptibility of Candida spp. - Trends over 10 years. J Infect. 2016;72(1):103-11. DOI: 10.1016/j.jinf.2015.09.041; PMID: 26518058
16. Lakoh S, Orefuwa E, Kamara MN, Jiba DF, Kamara JB, Kpaka S, et al. The burden of serious fungal infections in Sierra Leone: a national estimate. Ther Adv Infect Dis. 2021;8:20499361211027996. DOI: 10.1177/20499361211027996; PMCID: PMC8252340; PMID: 34262759
17. Hoenigl M, Seidel D, Sprute R, Cunha C, Oliverio M, Goldman GH, Ibrahim AS, Carvalho A. COVID-19-associated fungal infections. Nat Microbiol. 2022;7(8):1127-1140. DOI: 10.1038/s41564-022-01172-2; PMCID: PMC9362108; PMID: 35918423
18. Tang KWK, Millar BC, Moore JE. Antimicrobial Resistance (AMR). Br J Biomed Sci. 2023;80:11387. DOI: 10.3389/bjbs.2023.11387; PMCID: PMC10336207; PMID: 37448857
19. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard—Eleventh Edition. CLSI document M02–A11. Wayne: Clinical and Laboratory Standards Institute; 2012.
20. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: 30th Informational Supplement. CLSI document M100-S22. Wayne, Clinical and Laboratory Standards Institute; 2020.
21. Njunda AL, Nsagha DS, Assob JC, Kamga HL, Teyim P. In vitro Antifungal Susceptibility Patterns of Candida Albicans from HIV and AIDS Patients Attending the Nylon Health District Hospital in Douala, Cameroon. J Public Health Afr. 2012;3(1):e2. DOI: 10.4081/jphia.2012.e2; PMCID: PMC5345446; PMID: 28299076
22. Njunda LA, Assob JCN, Nsagha SD. Oral and urinary colonization of Candida species in HIV/AIDS patients in Cameroon. Basic Sci Med. 2013;2(1):1–8. DOI: 10.5923/j.medicine.20130201.01
23. Abrantes PMDS, McArthur CP, Africa CWJ. Multi-drug resistant oral Candida species isolated from HIV-positive patients in South Africa and Cameroon. Diagn Microbiol Infect Dis. 2014;79(2):222-7. DOI: 10.1016/j.diagmicrobio.2013.09.016; PMID: 24726686
24. Nweze EI, Ogbonnaya UL. Oral Candida isolates among HIV-infected subjects in Nigeria. J Microbiol Immunol Infect. 2011;44(3):172-7. DOI: 10.1016/j.jmii.2011.01.028; PMID: 21524610
25. Feglo PK, Narkwa P. Prevalence and antifungal susceptibility patterns of yeast isolates at the Komfo Anokye Teaching Hospital (KATH), Kumasi, Ghana. British Microbiol Res J. 2012;2(1):10–22. DOI: 10.9734/BMRJ/2012/861
26. David O, Ajayi YO, bablola TO. Virulence Factors and Antifungal Resistance in Dermatophytes Associated with Dandruff among University Students and a Tertiary Institution in Nigeria. Egypt Acad J Biol Sci G Microbiol. 2020; 12(2):1-8. DOI: 10.21608/eajbsg.2020.105965
27. Ungokore HY, Ehinmidu JO, Onaolapo JA, Olonitola OS. In Vitro Antifungal Susceptibility Profiles of Dermatophytes Isolates from Tinea Capitis in Northwest, Nigeria. Infect Epidemiol Microbiol. 2021;7(3):347-56. DOI: 10.52547/iem.7.4.347
28. Dongmo W, Kechia F, Tchuenguem R, Nangwat C, Yves I, Kuiate JR, et al. In Vitro Antifungal Susceptibility of Environmental Isolates of Cryptococcus spp. from the West Region of Cameroon. Ethiop J Health Sci. 2016;26(6):555-60. DOI: 10.4314/ejhs.v26i6.8; PMCID: PMC5389075; PMID: 28450771
29. Ayodele EH, Charles N, Abayomi F. Prevalence, identification and antifungal susceptibility of dermatophytes causing tinea capitis in a locality of north central nigeria. Afr J Infect Dis. 2020;15(1):1-9. DOI: 10.21010/ajid.v15i1.1; PMCID: PMC8047286; PMID: 33884353
30. Djohan V, Angora KE, Vanga-Bosson AH, Konaté A, Kassi FK, Yavo W, et al. [In vitro susceptibility of vaginal Candida albicans to antifungal drugs in Abidjan (Ivory Coast)]. J Mycol Med. 2012;22(2):129-33. DOI: 10.1016/j.mycmed.2011.11.005; PMID: 23518014
31. Eba M, Njunda AL, Mouliom RN, Kwenti ET, Fuh AN, Nchanji GT, et al. Onychomycosis in diabetic patients in Fako Division of Cameroon: prevalence, causative agents, associated factors and antifungal sensitivity patterns. BMC Res Notes. 2016;9(1):494. DOI: 10.1186/s13104-016-2302-1; PMCID: PMC5120551; PMID: 27876085
32. Maheronnaghsh M, Fatahinia M, Dehghan P, Teimoori A. Identification of Candida Species and Antifungal Susceptibility in Cancer Patients with Oral Lesions in Ahvaz, Southern West of Iran. Adv Biomed Res. 2020;9:50. DOI: 10.4103/abr.abr_214_19; PMCID: PMC7792871; PMID: 33457333
33. Arastehfar A, Wickes BL, Ilkit M, Pincus DH, Daneshnia F, Pan W, et al. Identification of Mycoses in Developing Countries. J Fungi. 2019;5(4):90. DOI: 10.3390/jof5040090; PMCID: PMC6958481; PMID: 31569472
34. Soriano A, Honore PM, Puerta-Alcalde P, Garcia-Vidal C, Pagotto A, Gonçalves-Bradley DC, et al. Invasive candidiasis: current clinical challenges and unmet needs in adult populations. J Antimicrob Chemother. 2023;78(7):1569-85. DOI: 10.1093/jac/dkad139; PMCID: PMC10320127; PMID: 37220664
35. Figueiredo TP, de Lucas RC, Cazzaniga RA, França CN, Segato F, Taglialegna R, et al. Antifungal Susceptibility Testing and Genotyping Characterization of Cryptococcus neoformans and gattii Isolates from HIV-Infected Patients of Ribeirão Preto, São Paulo, Brazil. Rev Inst Med Trop Sao Paulo. 2016;58:69. DOI: 10.1590/s1678-9946201658069; PMCID: PMC5048640; PMID: 27680174
36. May RC, Stone NR, Wiesner DL, Bicanic T, Nielsen K. Cryptococcus: from environmental saprophyte to global pathogen. Nat Rev Microbiol. 2016;14(2):106-17. DOI: 10.1038/nrmicro.2015.6; PMCID: PMC5019959; PMID: 26685750
37. Medina N, Alastruey-Izquierdo A, Mercado D, Denning DW, Arathoon E, Rodriguez-Tudela JL. Diagnostic Mycology Laboratories Should Have a Central Role for the Management of Fungal Disease. J Fungi. 2022;8(12):1285. DOI: 10.3390/jof8121285; PMCID: PMC9787327; PMID: 36547618
38. Mudenda S, Matafwali SK, Mukosha M, Daka V, Chabalenge B, Chizimu J, et al. Antifungal resistance and stewardship: a knowledge, attitudes and practices survey among pharmacy students at the University of Zambia; findings and implications. JAC Antimicrob Resist. 2023;5(6):dlad141. DOI: 10.1093/jacamr/dlad141; PMCID: PMC10733812; PMID: 38130703
39. Oladele R, Otu AA, Olubamwo O, Makanjuola OB, Ochang EA, Ejembi J, et al. Evaluation of knowledge and awareness of invasive fungal infections amongst resident doctors in Nigeria. Pan Afr Med J. 2020;36:297. DOI: 10.11604/pamj.2020.36.297.23279; PMCID: PMC7572690; PMID: 33117491
40. Johnson MD, Lewis RE, Ashley ESD, Ostrosky-Zeichner L, Zaoutis T, Thompson GR, et al. Core Recommendations for Antifungal Stewardship: A Statement of the Mycoses Study Group Education and Research Consortium. J Infect Dis. 2020;222(Suppl 3):S175-98. DOI: 10.1093/infdis/jiaa394; PMCID: PMC7403757; PMID: 32756879
41. Rabaan AA, Sulaiman T, Al-Ahmed SH, Buhaliqah ZA, Buhaliqah AA, AlYuosof B, et al. Potential Strategies to Control the Risk of Antifungal Resistance in Humans: A Comprehensive Review. Antibiotics. 2023;12(3):608. DOI: 10.3390/antibiotics12030608; PMCID: PMC10045400; PMID: 36978475
42. Kimbowa IM, Ocan M, Eriksen J, Nakafeero M, Obua C, Lundborg CS, et al. Characteristics of antimicrobial stewardship programmes in hospitals of Uganda. PLoS One. 2022;17(5):e0268032. DOI: 10.1371/journal.pone.0268032; PMCID: PMC9089898; PMID: 35536856
43. Adebisi YA, Alaran A, Badmos A, Bamisaiye AO, Emmanuella N, Etukakpan AU, et al. How West African countries prioritize health. Trop Med Health. 2021;49(1):87. DOI: 10.1186/s41182-021-00380-6; PMCID: PMC8547726; PMID: 34702370
44. Fang W, Wu J, Cheng M, Zhu X, Du M, Chen C, et al. Diagnosis of invasive fungal infections: challenges and recent developments. J Biomed Sci. 2023;30(1):42. DOI: 10.1186/s12929-023-00926-2; PMCID: PMC10278348; PMID: 37337179
45. Karajacob AS, Azizan NB, Al-Maleki ARM, Goh JPE, Loke MF, Khor HM, et al. Candida species and oral mycobiota of patients clinically diagnosed with oral thrush. PLoS One. 2023;18(4):e0284043. DOI: 10.1371/journal.pone.0284043; PMCID: PMC10109505; PMID: 37068057
46. Basu S, Copana R, Morales Jr R, Anugulreungkitt S, Puthanakit T, Maramba-Lazarte C, et al. Keeping It Real: Antibiotic Use Problems and Stewardship Solutions in Low- and Middle-income Countries. Pediatr Infect Dis J. 2022;41(3S):S18-25. DOI: 10.1097/inf.0000000000003321; PMCID: PMC8815843; PMID: 35134036
47. Osset-Trénor P, Pascual-Ahuir A, Proft M. Fungal Drug Response and Antimicrobial Resistance. J Fungi. 2023;9(5):565. DOI: 10.3390/jof9050565; PMCID: PMC10219139; PMID: 37233275
48. Li PKT, Chow KM, Cho Y, Fan S, Figueiredo AE, Harris T, et al. ISPD peritonitis guideline recommendations: 2022 update on prevention and treatment. Perit Dial Int. 2022;42(2):110-53. DOI: 10.1177/08968608221080586; PMID: 35264029
49. Wattal C, Chakrabarti A, Oberoi JK, Donnelly JP, Barnes RA, Sherwal BL, et al. Issues in antifungal stewardship: an opportunity that should not be lost. J Antimicrob Chemother. 2017;72(4):969-74. DOI: 10.1093/jac/dkw506; PMID: 27999053
50. Fisher MC, Denning DW. The WHO fungal priority pathogens list as a game-changer. Nat Rev Microbio. 2023;21(4):211-2. DOI: 10.1038/s41579-023-00861-x; PMCID: PMC9901396; PMID: 36747091
51. AMaghrabi RS, Al-Musawi T, Albaksami O, Subhi AL, Fakih RE, Stone NR. Challenges in the Management of Invasive Fungal Infections in the Middle East: Expert Opinion to Optimize Management Using a Multidisciplinary Approach. Cureus. 2023;15(8):e44356. DOI: 10.7759/cureus.44356; PMCID: PMC10539715; PMID: 37779746
52. Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-247. DOI: 10.1007/s00134-021-06506-y; PMCID: PMC8486643; PMID: 34599691
53. World Health Organization. WHO Global Strategy for Containment of Antimicrobial Resistance. Geneva; World Health Organization: 2001.
54. Pezzani MD, Mazzaferri F, Compri M, Galia L, Mutters NT, Kahlmeter G, et al. Linking antimicrobial resistance surveillance to antibiotic policy in healthcare settings: the COMBACTE-Magnet EPI-Net COACH project. J Antimicrob Chemother. 2020;75(Suppl 2):ii2-19. DOI: 10.1093/jac/dkaa425; PMCID: PMC7719409; PMID: 33280049
55. Seale AC, Gordon NC, Islam J, Peacock SJ, Scott JAG. AMR Surveillance in low and middle-income settings - A roadmap for participation in the Global Antimicrobial Surveillance System (GLASS). Wellcome Open Res. 2017;2:92. DOI: 10.12688/wellcomeopenres.12527.1; PMCID: PMC5645727; PMID: 29062918
56. McComick TS, Ghannoum M. Time to Think Antifungal Resistance Increased Antifungal Resistance Exacerbates the Burden of Fungal Infections Including Resistant Dermatomycoses. Pathog Immun. 2024;8(2):158-76. DOI: 10.20411/pai.v8i2.656; PMCID: PMC10939368; PMID: 38486922
57. Gow NAR, Johnson C, Berman J, Coste AT, Cuomo CA, Perlin DS, et al. The importance of antimicrobial resistance in medical mycology. Nat Commun. 2022;13:5352. DOI: 10.1038/s41467-022-32249-5
58. Bongomin F, Ekeng BE, Kwizera R, Salmanton-García J, Kibone W, van Rhijn N, et al. Fungal diseases in Africa: Closing the gaps in diagnosis and treatment through implementation research and advocacy. J Mycol Med. 2023;33(4):101438. DOI: 10.1016/j.mycmed.2023.101438; PMCID: PMC11103624; PMID: 38358796
59. Bahati F, Mcknight J, Swaleh F, Malaba R, Karimi L, Ramadhan M, et al. Reporting of diagnostic and laboratory tests by general hospitals as an indication of access to diagnostic laboratory services in Kenya. PLoS One. 2022;17(4):e0266667. DOI: 10.1371/journal.pone.0266667; PMCID: PMC8992978; PMID: 35395040
60. Stover KR, Hawkins BK, Keck JM, Barber KE, Cretella DA. Antifungal resistance, combinations and pipeline: oh my! Drugs Context. 2023;12:2023-7-1. DOI: 10.7573/dic.2023-7-1; PMCID: PMC10653594; PMID: 38021410
61. Beardsley J, Halliday CL, Chen SCA, Sorrell TC. Responding to the emergence of antifungal drug resistance: perspectives from the bench and the bedside. Future Microbiol. 2018;13(10):1175-91. DOI: 10.2217/fmb-2018-0059; PMCID: PMC6190174; PMID: 30113223
62. Niu X, Al-Hatmi AMS, Vitale RG, Lackner M, Ahmed SA, Verweij PE, et al. Evolutionary trends in antifungal resistance: a meta-analysis. Microbiol Spectr. 2024;12(4):e0212723. DOI: 10.1128/spectrum.02127-23; PMCID: PMC10986544; PMID: 38445857
63. Wulandari A, Hapsari R, Mujahidah, Sari D, Puspitasari I, Pramukarso DT. Antifungal susceptibility profile of Candida spp. causing candidemia in an Indonesian tertiary hospital. J Clin Microbiol Infect Dis. 2021;1(2):28-32. DOI: 10.51559/jcmid.v1i2.5
64. Seale AC, Hutchison C, Fernandes S, Stoesser N, Kelly H, Lowe B, et al. Supporting surveillance capacity for antimicrobial resistance: Laboratory capacity strengthening for drug resistant infections in low and middle income countries. Wellcome Open Res. 2017;2:91. DOI: 10.12688/wellcomeopenres.12523.1; PMCID: PMC5686477; PMID: 29181453
65. Fernandes R, Sabino R, Cunha C, Cornely OA, Carvalho A, Salmanton-García J, et al. Multicentric Study on the Clinical Mycology Capacity and Access to Antifungal Treatment in Portugal. Mycopathologia. 2024;189(1):15. DOI: 10.1007/s11046-024-00830-9; PMCID: PMC10808446; PMID: 38265528
Authors
Copyright (c) 2024 Abraham Bwalhuma Muhindo, Adamu Almustapha Aliero, Festo Mwebaze Syalhasha, Ibrahim Ntulume, Emmanuel Eilu, Martin Odoki, Joe Mutebi

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish in this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal the right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors can enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles (e.g., post-institutional repository) or publish them in a book, with acknowledgment of their initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process. This can lead to productive exchanges and earlier and greater citations of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.